HealthManagement, Volume 15, Issue 2/2013
Author
Alastair Gray
Health Economics Research CentreDepartment of Public Health University of Oxford
[email protected]
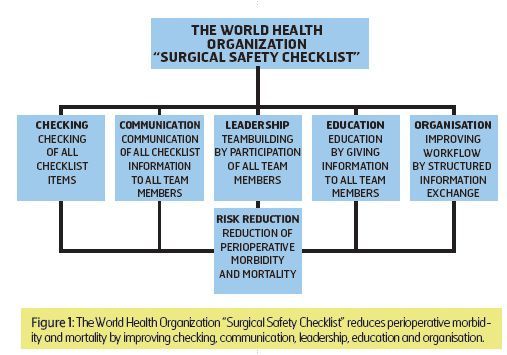
Hospital risk management includes human factors and technical hazards as well as leadership, procedural, educational, financial and organisational issues. The World Health Organisation’s Surgical Safety Checklist is a multifunctional risk management tool related to all these fields. The checklist reduces perioperative morbidity and mortality. However, its effectiveness depends on correct implementation and performance. Not only checking of important items, but also communication, teambuilding, leadership, education and organisation are important.
The Surgical Safety Checklist
The WHO Surgical Safety Checklist is a checklist designed to reduce perioperative mortality and morbidity by avoiding errorsand complications of surgery and anaesthesia. It consists of three parts, each containing roughly ten items concerning identity of patient and team members, anaesthetic and surgical procedures, preexisting diseases, equipment and postoperative recommendations. These items have to be checked and communicated orally to all participating team members at three points in time during the procedure.
The first point is immediately before induction of anaesthesia (Sign In), the second immediately before incision (Time Out)
and the third (Sign Out) immediately after suture. At these points in time the activity of all team members has to be interrupted to ensure that everybody is participating in communication.
The WHO checklist can be downloaded from the WHO website together with a guideline for implementation. Both correct
and incorrect practical application of the WHO checklist are demonstrated on videos accessible via YouTube.
The effectiveness of the WHO checklist on morbidity and mortality was first shown by Haynes et al. in 2008. These results led to a worldwide recommendation to use the checklist during all surgical procedures issued by the WHO and a number of studies confirming its effect on outcome and safety culture. These studies have been reviewed recently. This article focuses on the general principles of risk management involved in correct application of the WHO checklist and their impact on implementation.
A Multifunctional Risk Management Tool
Human Factors
Risk management must take into account human factors, communication, equipment and processes as well as leadership, procedural, organisational, financial, and educational issues. Implementation and use of the WHO checklist is related to all these fields (Figure. 1). Human factors have been recognised as primary sources of complications and critical incidents in medicine as well as in other critical environments in industry and transportation. Lack of knowledge and skills, errors, mistakes and mishaps are causes of false actions and thoughts resulting in adverse events. These individual errors can be reduced by checking important issues using the WHO checklist.Communication
In addition to individual human errors, communication problems have been identified as a major cause of complications in medicine. Bad communication habits increase the risk of complications due to loss of important information. Hence, understanding and using the WHO checklist as a communication tool is essential for its effectiveness.This aspect is not always easy to realise in practice. Speaking up and repeating all important aspects loud and clearly to all team members is unfamiliar to many operating room staff members and sometimes regarded as redundant and too time consuming. Using the checklist is often reduced to ticking all the boxes by one team member without communicating with others. Therefore training and supervising the application of the checklist in clinical practice are important parts of implementation. This is achieved, if one team member with sufficient authority supervises and corrects errors during the use
of the checklist.
Equipment
Equipment problems and technical hazards are rare in comparison to human failure. However, they are regarded as more avoidable than the latter by defined interventions. Confirming functioning of technical devices and completeness of instruments are parts of the three points in time of the WHO checklist. Procedural standardisation is another importantissue. Local written and standardised procedures referring to national or international guidelines are recommended to reduce perioperative risk. The WHO checklist is a standardised protocol and operating theatre workflow is facilitated by the clear communication structure provided.
Leadership
Leadership style also has a substantial impact on team performance, error rates and patient outcomes. Top-down attitudes combined with misconduct, intimidating or disruptive behaviour negatively affects the mood and well-being of co-workers. Moreover, it increases error rates and impairs patient outcomes in the operating room. Leadership in medicine is widely regarded as a soft skill that cannot be taught or influenced by systematic approaches. However, there is a lot of available literature on leadership and some basic principles can be learned quickly.Good leaders have an equally high goal and people orientation, thus keeping a balance between the requirement of achieving a task and good interpersonal relationships. They prefer a flat hierarchy with short lines of communication. Performing the WHO checklist systematically enforces good leadership habits like contacting and informing all team members about what is planned and what background information is needed as well as providing time for remarks and questions without disturbing the procedure.
Intentionally including all team members in information exchange regarding the upcoming common task during Sign In and Time Out enforces teambuilding, thus improving motivation and performance. Sign Out functions not only as an information exchange about the completed procedure and postoperative orders, but also provides an opportunity for a short team debriefing including critical incident reporting, if needed. In complicated cases this is an opportunity to arrange a postoperative meeting to debrief the case systematically. The item “Criticism or suggestions for improvement” can be added to the WHO checklist to provide an opportunity to communicate remarks about problems during the case without interfering at an inappropriate point in time during surgery.
Financial Factors
Risk management is connected with financial management, since from the financial point of view cost effectiveness of risk reducing procedures has to be proven to justify the expenses. However, cost-cutting has been regarded as a threat to risk management. It leads to potentially dangerous production pressure with the requirement to treat more patients in less time with fewer personnel. The WHO checklist has repeatedly been criticised for being too time consuming and therefore costly, albeit its positive effect on outcome has been shown by several studies and the expenditure of time is relatively low (less than two minutes per surgical procedure). Moreover, a recent study has shown that the spending saved by avoidingcomplications probably exceeds the costs of implementation and performing the WHO checklist in most hospitals.
Education
Improving education of personnel with special emphasis on safety topics and human factors is a further means to reduce the risk of perioperative complications. Education is improved by using the Sign In, Time Out and Sign Out to explain the surgical and anaesthesiological procedure and postoperative recommendations to all team members. In university hospitals there is nearly always at least one medical or nursing student in the operating theatre who does not have all the information that is needed to understand the surgical and anaesthesiological approach.Implementation
Implementation of the WHO checklist needs to be organised systematically to guarantee successful adoption. It is not sufficient to release a copy of the original WHO checklist and simply order its use without thorough preparation, information, training and supervision of its application. First, it has to be checked, whether the original WHO checklist is applicable to the hospital without changes of language and content. After translation, the contents have to be adopted to include important features that are not part of the original WHO checklist or omit items that are not applicable for the hospital. For example, checking for massive blood loss is not important in ophthalmology and can therefore be omitted in a hospital specialised in eye surgery. Otherwise, it has to be avoided to include too many additional items, since overloading the list renders its application more time consuming and reduces its acceptance.An adopted checklist may not include the WHO logo but it must contain the reference: 'Based on the WHO Surgical Safety Checklist, URL, http://www.who.int/patientsafety/safesurgery/en, © World Health Organization 2008 All rights reserved. The adopted WHO checklist has to be sent to the WHO to authorise its use.
The checklist can be adapted by reducing the questions to key words and omitting the tick boxes to reduce reading time and to focus more on the correct performance than on ticking the boxes. A detailed, but short handout should be written to inform all staff members about the procedure. However, in practice most staff members have to be informed by oral instruction either personally in the operating theatre or by lectures on the WHO checklist of about 45 minutes preferably including videos demonstrating the correct application. It is important to arrange enough time for discussions during the lectures. The WHO checklist should be first implemented in one operating theatre for some weeks to demonstrate its practicability.
Implementation of the WHO checklist should be accompanied by other measures of risk management concepts including other perioperative checklists (e.g. for preparation on the ward or handover in the recovery room), the ABCDE-system for critical incident management and systematic communication, a critical incident reporting system (CIRS) and safety rounds.
The Checklist Concept Outside the Operating Theatre
The WHO checklist concept of interrupting workflow for effective communication can also be integrated into team procedures outside the operating theatre. Trauma resuscitation room management is an example. A Sign In can be performed before arrival of the patient in the resuscitation room consisting of (Sheffield) could not provide information on discharge dates of patients. As a result, the economic analysis was conducted using 291 patients on antibiotics in five hospitals. Summary data are given in Table 1. The main specialties were general medicine (n=134, 46%) or general surgery (n=91, 31%). Patients were mainly living with their family (61%) or alone (27%). Average age when assessed was 69 years, and 29% of the sample were aged 80 or older.A summary of the results of the assessment is given in Figure 1. 82 patients (28%) were assessed as suitable for discharge,
of whom 54 (66%) were on oral antibiotics and 28 (34%) on IV antibiotics; in 4 instances earlier discharge would only have been feasible if Outpatient Parenteral Antibiotic Therapy (OPAT) services were available. In total, 150 (51%) of the 291 patients assessed were considered suitable for stopping or switching their current antibiotic therapy.
The costs and savings from these proposed therapy changes are reported in Table 2. The reduction of 494 in-patient days arising from earlier discharge would have saved £186, 731. Savings from switching from oral to no antibiotic would have been small, but, £10, 536 would have been saved by switching from IV to no antibiotic, and £9, 233 from switching from IV to oral therapy. There would also have been some additional costs: the clinical assessment would have cost £2, 468, community support would have cost £6, 227, and OPAT services would have cost £5, 616. In total, the net effect of these changes would have been a potential saving of £192, 635, equivalent to £662 (95% c.i. £393, £930) per patient in the study.
Sensitivity Analyses
Some patients had long lengths of stay which may have had a large influence on the total number of bed-days and potential days saved. To assess their effect, the eight patients having the largest impact on potential bed-day savings were excluded from the analysis: this resulted in savings falling to £363 per patient, but this remained highly significant (95% c.i. £261, £465). Similarly, increasing or decreasing by 25% the assumed cost of providing an OPAT service (£151.8 per person per day) had little effect on the overall results, changing the net saving per person to £667 or £657.If the number of patients deemed suitable for early discharge was only 50% of the baseline assumption described above, the net saving per patient would fall to £260. Finally, if 10% of the patients deemed suitable for early discharge had to be readmitted, net savings per patient in the study would fall from £662 to £529.
Discussion
In this study the objective was to quantify the potential benefits in economic terms of an antibiotic review and early discharge assessment. Using data collected in a wide range of different hospitals and specialties and for a range of patients, the study found that 28% of patients assessed could be suitable for early discharge, and that another 23% of patients could have had their current antibiotic treatment either stopped or reduced. Conducting such an assessment, and providing some additional out of hospital support services, would of course involve some added costs, but these would be just a small fraction of the potential savings. Reductions in lengths of stay arising from earlier discharge were the main source of potential savings.In practice, in-patient days saved might not result in cash savings, but from an economic perspective they can be viewed as opportunity costs: earlier discharge of some patients may allow waiting times for other patients to be reduced, for example.
While the potential savings from such a scheme would mainly benefit hospitals, the additional costs involved would fall mainly on community service budgets. Service commissioners would need to recognise these issues to ensure fair outcomes and correctly aligned incentives. Similarly, early discharge schemes could reduce costs falling on the formal health services, but increase the burden on family and friends. This study was unable to collect information on such issues, which would be a valuable focus for further research.
If such interventions were being fully evaluated, they would also have to take into account their impact on health outcomes
such as quality of life. Recent years have seen other initiatives to improve antibiotic stewardship, such as self-assessment toolkits. But many audits and official reports still proclaim the need for improved antibiotic management. Focusing on the potential cost savings reported in here as arising from formal antibiotic review might increase the incentive to introduce such policies.
Finally, the pressure to innovate would be enhanced by evidence from randomised trials or case-control studies: the results reported here are illustrative and need to be confirmed in a rigorous experimental study design, but they do suggest that such a study might well be worthwhile.


![Tuberculosis Diagnostics: The Promise of [18F]FDT PET Imaging Tuberculosis Diagnostics: The Promise of [18F]FDT PET Imaging](https://res.cloudinary.com/healthmanagement-org/image/upload/c_thumb,f_auto,fl_lossy,h_184,q_90,w_500/v1721132076/cw/00127782_cw_image_wi_88cc5f34b1423cec414436d2748b40ce.webp)


