HealthManagement, Volume 14, Issue 3 /2012
After quality management made its entry into the healthcare system at the beginning of the 1990s, triggered by the commodification of the medical and care sector, the year 2000 saw the establishment of risk management with the aim to lower complication and loss rates. For several years now, movement and further development has been recognisable. The patients themselves, as a target group of service provision in healthcare, are calling for not only good quality diagnostics, therapy and care but also a high level of safety. The error of comparing quality, risk and patient safety management should be avoided. All three concepts are strongly connected to each other and are logical extensions of one another. Clinical risk management (cRM) operationalises quality management and patient safety management substantiates and specifies risk management focusing on the addressee of service.
There are still relatively few studies on the degree of implementation of risk management measures in German hospitals. The DKI hospital barometer 2008 showed that the vast majority of clinics have only recently started to be concerned with the development of clinical risk management and are still a long way from implementation. A 2010 study carried out by order of the Institute for Patient Safety (IfPS) concluded that German hospitals have become more active with regard to prevention (case conferences, risk audits, full-time employees), but that there are still many development potentials.
Critical Success Factors of Clinical Risk Management
Like other activities which bind to a high extent human and organisational resources it is important to concentrate on the essential contents. The following six point proposal may contribute to promote an efficient use of resources and, in particular, to motivate employees to get involved.
1. The cRM shall consider relevant safety problems
Worldwide, there are various initiatives aimed at promoting patient safety. According to the "High Five" Recommendations of the World Health Organization (WHO), global measures • For managing concentrated injectable medicine;
• For assuring medication accuracy at transitions in care;
• Communication failures during patient handovers;
• Addressing healthcare-associated infection; and
• For performance of correct procedure at correct body site are action fields which have to be treated with high priority. The German Action Group Patient Safety (APS) developed clear and pragmatic recommendations for promoting patient safety, for example to avoid leaving unintentionally foreign objects in the surgical field or wrong site surgery, for secure patient identification and for medication therapy safety.
However, a glance into the error in treatment registers of the insurance sector shows that the prevention measures outlined above do not cover the entire spectrum of the causes of loss. Illustration 1 shows the distribution of causes considering 110,000 claims which were handled by Ecclesia Versicherungsdienst GmbH. It is obvious that diagnosis and therapy errors represent the most frequent causes of errors in treatment. Prevention measures such as mortality and morbidity conferences, inter-professional diagnosis and indication checks (e.g. in the tumour board) and interdisciplinary evaluations of treatment results are of incomparable usefulness and paramount importance.
2. Patients should be involved in the development of patient safety
The processes in medicine and care have become more complex, technologies have become more sophisticated and the patient himself has become considerably more critical as compared to 20 years ago. In other production and service sectors it therefore seems reasonable to involve the recipient of services in controlling and development. The WHO has taken the initiative with the project "Patient for Patient Safety" in 2004, and sponsors projects for the "Patient Empowerment". In the meantime, there are specific survey instruments for patients available, which are specifically aimed at patient safety (e.g. PaRiS- Patient Risk and Safety survey of the research group Metric in Germany). The Austrian platform Patient Safety and the Foundation Patient Safety in Switzerland have developed information booklets which inform the patient about his/her cooperation possibilities for promoting his/her safety already at hospital admission.
The Klinikum Altenburger Land finished and published a patient safety movie in October 2011. In a six minute video which the patient receives on admission, which is also shown on the hospital's website and will be soon shown on screens in the waiting zones, patients learn what is done for their safety, what previously remained hidden to them: The counting control in the OR, the cardiopulmonary supervision in the onguard- room or ensuring the right medication. The presented examples are highly suitable to involve the patient in the safety process and to promote an atmosphere of confidentiality.
3. The aims and initiative of the cRM need to be communicated
The measures for the promotion of patient safety and for clinical risk management are usually very varied. The department for anaesthesia uses, for example, the Critical Incident Reporting System for its special branch, the employees of the care team work with international grading systems for a care diagnosis without coordinating these with the medical service, or the physiotherapy department develops standards for fall prevention without any lasting networking in the therapeutical team. For developing effective prevention structures it is necessary to introduce system networking like in all other areas. Intranet portals on institutional level are of great benefit here. A broad inter-professional participation in the systems is essential.
4. Suitable instruments need to be applied in the cRM
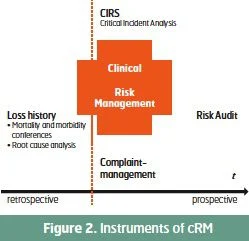
Different instruments and methods of working are available. In principle, these should actively support the RM process in all phases of risk identification, assessment, management and control. Different instruments interfere at specific points in this process, and complement one another with regard to the effect. The impact is such that safety vulnerabilities are identified, and, based on this, preventive measures may be initiated. Retrospective procedures are aimed at analysing events of the past. So a root cause analysis or the mortality and morbidity conference are used for the retrospective analysis of actual loss events. The Critical Incident Reporting System (CIRS) and a complaint or feedback management system are focused on actual medical processes: Errors not involving damage and patient complaints are assessed as simultaneously as possible to the treatment process. The analysis of such errors and occurrences leads to the development of prevention measures. Prospective instruments aim at preventing loss events before their emergence by classifying high-risk workflows or structures with regard to the probability of loss occurrence and the potential extent of loss. Scenarios are developed and analysed with the help of safety and risk audits in order to derive suitable prevention measures from it. It is one of the primary tasks of those responsible for the cRM to make a situation-specific and targeted use of these different instruments and methods.
5. The effects of prevention measures need to be measured
cRM procedures call for a high level of involvement of physicians and nurses and also considerable financial resources. In this context it is especially important to measure the effect of the corresponding measures. In this respect, a lot has been done in recent years. For the last five years results of studies which explicitly address the topic of patient safety have been published. Pointing the way ahead was probably the study of Haynes from 2009 for the introduction of a Surgical Safety Checklist, with which the effect of using an OR check list could be proved. The mortality rate stood at an average level of 1.5% before the introduction, and after that it lowered to approx. 0.8%. The complication rate could be reduced from 11% to 7%. Now, this check list (surgery preparation/team-timeout/ postoperative care) is used in many operating theatres in German-speaking countries, often in a tailored version. In 2008, Steyrer analysed the safety culture in hospitals in Austria. Employees were questioned to assess the safety culture of nine specialist departments using the Viennese safety culture questionnaire. Six departments were examined in which RM audits were carried out and a critical incident reporting system (CIRS) was introduced and also three departments without any audits or CIRS. The questionnaire was distributed in a phase before the risk audit and in a defined phase after the evaluation audit. At the same time, the questions were also asked in non-CIRS departments. The CIRS group considerably improved in the following categories:
• Communication and cooperation with respect to patient safety;
• Attitude towards error management;
• Personal acceptance of responsibility;
• Assessment of the initiated safety efforts; and
• Knowledge of specific problem areas.
In as much as patient safety and cRM become the subject of scientific research internationally, before its introduction every single hospital needs to define when and by what methods the projects shall be evaluated. The institutions owe it to their patients and employees to be able to make a statement on whether the error rate decreased due to the introduction of CIRS or whether the complication rate could be reduced due to the the establishment of a mortality and morbidity conference. The results of studies and examinations on the effect of cRM show that six target levels can be reached. It promotes patient safety, serves the organisational development, sensitises the therapeutical team in terms of risks, supports inter-professional communication and cooperation, creates legal certainty, and provides the prerequisites for the insurability of the respective institution.
6. The conditions must be developed and promoted
Patient safety requires a safety culture. Pfaff defines this as an institution's stock of knowledge, values and symbols, which increases its capacity to promote safety. It concerns the provision of knowledge and skills and also the development of standards and rules of conduct. In addition, the institution needs to define safety as a special "value in itself".
Hoffmann and Rohe accurately classified five levels of maturity of a safety culture:
Negative safety culture (level of maturity 1): Patient safety is considered only hesitantly. When critical events occur, guilty persons are searched and sanctioned. Learning from errors does not take place.
Reactive safety culture (level of maturity 2) The organisation only takes action when critical events occur.
Correct safety culture (level of maturity 3) Quality and risk management models and systems are complied with due to pressure of external guidelines.
Pro-active safety culture (level of maturity 4) Measures for the increase of patient safety are initiated without any critical events having occurred.
Trend-setting safety culture (level of maturity 5) Patient safety is a self-evident and routine part of work for all persons working in the organisation.
Many institutions are currently still in a condition between level 2 and 3. However, many occupationhospitals have already set out to reach level 4 or even 5 by introducing and establishing suitable systems and instruments.
Conclusion
We have achieved so much for the development of clinical risk management and for the promotion of patient safety within the last 10 years. However, there is still considerable potential for development. A great concern is the patient's perception. The patient is increasingly uncertain despite all inner clinical developments. Recent studies show that patients are particularly afraid of hospital infections. The media has played a part in this "uncertainty perception". Robert Wächter accurately says in his book "Understanding Patient Safety" published in 2008:
"Patient safety could be increased enormously. But we should not rest, until patients exclusively come into our care with fears and worries about their illness and possible consequences. They should not have any fears and worries, about suffering damage or even dying from a medicine, which was actually intended to help them. There is still a long way to go!"
Clinical risk and patent safety management is no longer a voluntary exercise but a "must-have programme" for every hospital. Patient safety also contributes to brand development in the growth market healthcare, and it is a business management option since hospitals are better insurable with an established RM. But first and foremost the service providers owe it to the patients. Patient safety is a patient right and the obligation of all members of staff.


References:
References available upon request, [email protected]