HealthManagement, Volume 10, Issue 1 /2008
Towards managerial and financial convergence
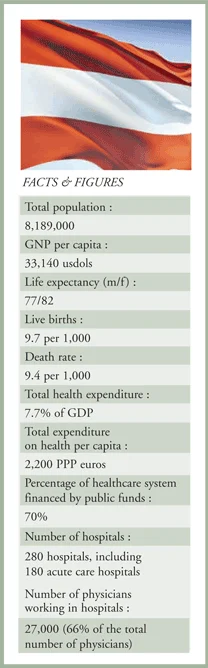
Austria is a democratic republic and a federal state which is composed of nine Länder. The Länder have their legislative competencies and also participate in legislation at a federal lervel in the Bundesrat (upper house of parliament).
Health System Structure
The Austrian healthcare system is characterised by the federalist structure of the country, the delegation of competencies to self-governing stakeholders in the social insurance system as well as by cross-stakeholder structures at federal and Länder level which possess competencies in cooperative planning, coordination and financing. According to the Federal Constitution, almost all areas of the healthcare system are primarily the regulatory responsibility of the federal government. The most important exception is the hospital sector. In this area, the federal government is only responsible for enacting basic law; legislation on implementation and enforcement is the responsibility of the nine Länder.
The various sectors of the healthcare system have traditionally been characterised by different stakeholders and regulation- and financing mechanisms. However, in recent years there have been increased efforts to introduce decision- making and financing flows which are effective across all sectors. Since 2002, all the Länder, except Vienna, as well as some of the private nonprofit owners, have privatised their hospitals, mainly in the form of organisational privatisations. The various private operating companies have one thing in common: they are responsible for the management of hospitals, whereas the Länder or local authorities as (majority) owners usually act as a guarantor. The Austrian healthcare system has developed almost completely into a model which is mainly based on decentralised contracts with all service providers.
Healthcare Financing
The financing of the healthcare system is pluralistic in accordance with the constitution and social insurance laws. The social health insurance system, which is the most important source of financing, provided a total of 45,3% of total healthcare expenditure in 2004. Mandatory insurance is based on membership of an occupational group or place of residence; thus, there is no competition between health insurance funds.
25% of total healthcare expenditure is financed by the federal government, the Länder and local authorities. 10% of this share was accounted for by tax financed long-term care cash benefits. The latter have been paid out to people in need of long-term care since 1993.
In 2004, around 25% of healthcare expenditure was financed privately. Private households bore 13,5% of healthcare expenditure by means of indirect cost-sharing (services whose costs were fully borne by the insured) and 7,6% by means of direct cost sharing (co-payments). Direct cost sharing was increased in recent years and affects almost every service provided by social health insurance; however, the outpatient clinics fee introduced in 2001 was withdrawn again in 2005 due to the high costs involved in its implementation and the considerable resistance it had encountered.
Delivery System
Those covered by health insurance can freely choose between service providers in the outpatient sector, of whom the majority work in individual practices. In addition, outpatient clinics and hospital outpatient departments offer outpatient care. Compared to 1980, the number of practising physicians and dentists has risen at an over-average rate, with the figures for both professions actually doubling. There is a considerable variation in the density of physicians between the Länder. The number of nursing staff also doubled between 1980 and 2003 to 6 per 1000 inhabitants. However, it was still clearly below the EU average of 7,3 in 2003.
Hospitals which are listed in the hospital plan of a Land are subject to public law (“fund hospitals”) and have a statutory requirement to provide care and to admit patients. They are entitled to legally prescribed subsidies from public sources for investments, maintenance and running costs. The ratio of beds to inhabitants of 6,1 beds per 1,000 persons is clearly above the EU average. The average length of stay, 6 days is shorter than the EU average, the utilisation of bed capacity at 76% marginally below.
With the passing of the 1993 Federal Long-Term Care Act, Austria reacted comparatively early to the approaching demographic challenges. Like acute inpatient care, long term care too is a sector where federal cooperation instruments are used, specifically to ensure the uniformity of entitlement criteria and quality standards of long term care institutions.
Health Reforms
Health reforms have primarily dealt with cost containment (by exploiting potential for more efficiency and raising cost sharing) and with structural reforms to improve the planning of capacities, the cooperation of stakeholders and the coordination of financing flows.In the acute hospital care sector organisational privatisations were performed which was essentially completed by 2002. The reimbursement of services and medicines by social health insurance has been more strongly linked to health technology assessment, but only a small number of benefits have been excluded. At the same time, new benefits have been introduced, such as federal long term care benefit, psychotherapy, preventive services, and new structures for community-based long term care.
Contribution revenue has increased and the contribution rates of some groups of the insured brought into line, but the revenue base has not fundamentally changed. Quality assurance requirements have been raised and patients’ rights have been strengthened by a charter and patients’ ombudpersons.
DRG System
The Austrian DRG system of hospital financing is developing. Its main focuses are the inclusion of the promotion of day care services and the updating of the model through calculations using a revised calculation guide based on updated hospital cost accounting. Furthermore, integrated supply concepts and the reduction of the burden on inpatient care are to be promoted by the development of a points model for medical follow-up care, transfers between departments and hospitals, and readmissions. The coordination of the Austrian DRG model with the services supplied in hospital outpatient departments and private practice is to be achieved through the harmonisation of documentation and the separation of the contents and the scoring of flat rates per case from other areas of care provision. In addition, a performance-orientated financing concept is to be developed for the outpatient sector which is coordinated with the inpatient sector.
The creation of a new instrument of cooperation designed to provide motivation for cooperation between financing bodies is closely linked to the structure of raising funding for hospital financing. Important impulses for cost-containment will result from this cooperation if the stakeholders involved interact in a constructive manner. Conclusion In the past 25 years, the stakeholders in the Austrian healthcare system have succeeded, characteristically by means of cooperative agreements and planning, in ensuring almost universal healthcare provision with a comprehensive benefit catalogue, in spite of considerable increases in expenditure and continuing cost containment measures.
Waiting times for medical treatment are rarely discussed in public and can be viewed as short in comparison to other countries, although there has been no precise evaluation of this. However, the supply structure is characterised by inequalities between the Länder and also between urban and rural areas. Altogether, life expectancy and most of the documented health indicators have improved markedly in the past 15 years. The level of satisfaction of the population with the healthcare system continues to be high in an international comparison.
Sectoral fragmentation, which also creates bias towards hospital care, is a long standing weakness of the Austrian healthcare system. In spite of numerous efforts, it has until now not been possible, in the sense of allocative efficiency, to allow funding to follow the services provided across sectoral borders. Nor has it been possible to structure the supply chain in a more needs-orientated way across these administrative and financial barriers at the sectoral borders, especially between outpatient and inpatient care or acute and long-term care.
The planning, structures and funds introduced since 2005 permit for the first time the cross-sectoral steering of capacities and financing flows. They also provide for incentives for improved interface management and integrated forms of care.


![Tuberculosis Diagnostics: The Promise of [18F]FDT PET Imaging Tuberculosis Diagnostics: The Promise of [18F]FDT PET Imaging](https://res.cloudinary.com/healthmanagement-org/image/upload/c_thumb,f_auto,fl_lossy,h_184,q_90,w_500/v1721132076/cw/00127782_cw_image_wi_88cc5f34b1423cec414436d2748b40ce.webp)