HealthManagement, Volume 15 - Issue 1, 2015
In accordance with the objectives of the Quality, Innovation, Productivity and Prevention (QIPP) programme, our innovative solution of outsourcing work to a commercial community partner without significant upfront funding has enabled NBT Pharmacy to provide a high quality service and manage a doubling workload within existing budgetary constraints.
Background
Compliance aids
Compliance aids are “Multi compartment compliance aids” (MCAs) often called “blister packs”. They are medicine storage devices that usually contain 7 days of medication and act as a reminder for patients to take their medicines, enabling them to manage their own often complex and confusing drug regimens.
We continue to have an ageing population and more people that need supporting in their own homes, so the issue of supplying compliance aids is an increasing one.
MCAs can support some patients to remain in their own homes longer, reducing some need for residential care. Providing medication in an unsuitable format leads to patient confusion/medication errors. The National Patient Safety Agency highlights that medication errors can cause harm to patients, and can lead to increased morbidity/mortality, inflated healthcare costs and hospital re-admissions (National Patient Safety 2007; 2009).
MCAs also act as a visual prompt for carers, indicating that patients have taken their medicines, or at least removed them from the device. Nationally, the need for compliance aids is increasing, reflecting the ageing population and an increase in complexity and average numbers of drugs taken.
The supply of MCAs is a national issue throughout pharmacies, both in hospitals and in the community. MCAs are NOT the answer to all medication issues but are suitable if patients are assessed appropriately

Figure 1. Example of an MCA
NBT
Our work started when NBT was a large Acute Teaching Trust on two sites with approximately 1000 beds, 53 wards and 9000 staff. Despite implementing an assessment tool to minimise inappropriate use of compliance aids, the demand for their dispensing has doubled during the last five years to over 200 per month, exceeding capacity and causing:
- Delayed discharges;
- Inappropriate discharges (when medication was not supplied in a compliance aid) causing problems in primary care and possible re-admissions;
- Non-compliance;
- Complaints (from GPs, patients and relatives).
Various service improvements and actions at NBT did not enable capacity to meet demand. We realised that we could not solve the issue in house and needed to explore outsourcing options.
In 2007 NBT became involved in the Safer Patients Initiative (SPI2): 2007 – 2009 and then the Southwest Quality and Patient Safety Improvement programme: 2009 – now Safer Care South-West. The Safer Patients Initiative was a programme developed by the Institute of Healthcare improvement (IHI) and the Health Foundation (HF).
At the end of May 2014 we moved into a new hospital on one site with approximately 850 beds and 27 ward areas.

Figure 2. New Southmead Hospital: May 2014
Rationale behind usage
Drivers influencing usage include:
- Disability Discrimination legislation (Disability Discrimination Act 1995; 2005 - Equality Act 2010) requires that pharmacists and dispensing practices should make “reasonable adjustments” to enable disabled persons to use their medicines.
- The National Institute for Health and Clinical Excellence (NICE) clinical guidelines (National Institute for Health and Clinical Excellence 2009) and Cochrane Review (Mahtani et al. 2011) both suggest MCAs may be of value in patients who have been assessed as having practical problems in managing their medicines.
- The Royal Pharmaceutical Society (RPS) report (Picton and Wright 2013) on Medicines Optimisation has four key principles including:
- Principle 1 - Aim to understand the patient’s experience.
- Principle 3 – Ensure medicines use is as safe as possible.
- The
second RPS report Improving patient
outcomes: the better use of multi-compartment compliance aids (Royal
Pharmaceutical Society 2013) is aligned to the principles of medicines optimisation
and says that MCAs may be useful as a support system.
- The NHS England Patient Safety Alert Risks arising from breakdown and failure to act on communication during handover at the time of discharge from secondary care also highlights the importance of medicine use and safety (NHS England 2014).
The decision to outsource from NBT’s perspective was primarily patient-focused. We started our work to support patients who needed MCAs back in 1998. At that time, we were not supplying MCAs, but recognised that if medication was not dispensed in suitable containers, then some patients may not be able to manage their medicines, and may have to be re-admitted very quickly.
Before this project the demand for the dispensing of compliance aids doubled over five years, This exceeded in-house capacity and caused;
- Delayed discharges;
- Inappropriate discharges;
- Complaints.
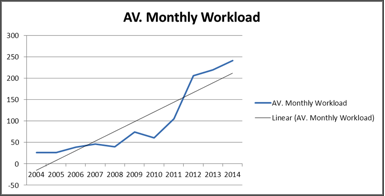
Figure 3. Average Monthly Workload
Figure 3 shows how our average monthly workload has continued to grow from 2004 to 2014.
Aims and Objectives
The aim of this initiative was to improve the provision of compliance aids in accordance with the objectives of the Quality, Innovation, Productivity and Prevention (QIPP) programme by:
- Managing the increasing workload;
- Reducing discharge waiting times;
- Reducing length of stay;
- Supporting patients to manage medicines at home and reduce some need for residential care.
Method
NBT Pharmacy devised a phased and innovative solution that did not require significant upfront funding by outsourcing the work to a commercial community partner – LloydsPharmacy and the wholesaler AAH Pharmaceuticals (parent company Celesio). This evolved from a mixed service of both in-house dispensing and supply through negotiation with community pharmacies, to outsourcing work.
We achieved our results with the use of the Model for Improvement and Plan, Do, Study, Act (PDSA) cycles and tests of change on one ward. We established ongoing tests of change with ongoing measurement.

Figure 4. PDSA cycle (Plan, Do, Study, Act)
Source: NHS Institute for Innovation and Improvement 2008 (Quality and Service Improvement Tools)
Phase 1: Feb 2009 – June 2010
We piloted “small tests of change” with a LloydsPharmacy community branch to provide a dispensing service for Southmead Pharmacy against a service level agreement. All prescriptions were clinically screened by an NBT pharmacist before faxing to LloydsPharmacy.
Turnaround time ranged from 22–46 hours. Southmead received daily weekday deliveries by a LloydsPharmacy driver. Time was taken to embed practices. The pilot was successful, but demand for this service rapidly exceeded capacity within the branch.
Phase 2: July 2010 – Aug 2010
Dispensing transferred to the central AAH premises in Bristol (“The Hub”), who sub- contracted dispensing to LloydsPharmacy. Prescriptions from NBT were scanned and emailed to “The Hub”. AAH carried out deliveries via their usual van fleet.
Phase 3: Sept 2010 – Jan 2011
The service extended to Frenchay Pharmacy.
Phase 4: Feb 2011 – Sept 2012
There was an increase in deliveries, including Saturdays. Southmead Pharmacy continued to pack in house for discharges required at short notice. Skill mix was introduced in the form of Band 4 technicians to release pharmacists’ involvement with the Hub. Regular review meetings were held to discuss progress and developments.
Phase 5: Oct 2012 – present time
The outsourcing was further enhanced by the introduction of a “Golden Patient” service, which enabled a same day turnaround of 4.5 hours (Reserved for short stay wards only).
Compliance aid data is collated on a monthly basis eg workload, dispensing/delivery errors, wastage of medication. Wastage is a fine balance between dispensing in a timely fashion to avoid delaying discharge versus the possibility of medication changes.
Results
Table 1 shows the overall results from the phases:
Phase | Description | Turnaround | Monthly Rate (Average) | Monthly Rate (Peak) | Duration |
Pre-Pilot | Performed in house | N/A > 48 | 34 | 40 | 12 Months |
Phase 1 | Pilot with LloydsPharmacy Community Branch | 22-46 | 50 | 74 | 18 Months |
Phase 2 | Pilot with managed central service provided by The Hub | 21-45 | 56 | 61 | 2 Months |
Phase 3 | Service extended to both NBT sites | 21-45 | 80 | 105 | 5 Months |
Phase 4 | Service levels increased to reduce maximum turnaround time | 21-26 | 141 | 206 | 20 months |
Phase 5 | Golden patient service introduced for limited patients | Golden patient 4.5 Normal patient 21-26 | 210 (includes 25 Golden pts) | 280 (includes 42 Golden pts) | 27 months |
Table 1. Overall Results from the Phases
The main impacts of our work are shown by how we have managed an increase in demand and the impact on patients’ waits (ie turnaround times):
Monthly workload and Turnaround times
Phase 1
· Average: 50 MCAs
· Turnaround time: 22-46 hours
Phase 5
· Average: 210 MCAs
· Turnaround time: 21-26 hours
· (4.5 hours for “Golden Patients”)
We managed a 300 percent increase in demand.
Phase 1
· Average: 50 MCAs
Phase 5
· Average: 210 MCAs
· 94% of MCAs are now dispensed by “The Hub”
· (13% “Golden Patients”)
This is more easily seen in the following increases in monthly workload graphs showing different aspects of the work:
· Figure 5 – monthly workload for NBT: normal vs “golden patients”
· Figure 6 – monthly workload for NBT: phase 1 vs phase 5
· Figure 7 - monthly workload for NBT: Hub vs in house
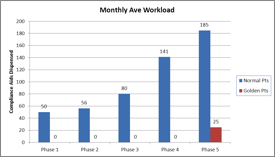
Figure 5. Average Monthly Workload for NBT
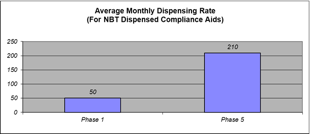
Figure 6. Average Monthly Workload for NBT: Phase 1 And 5
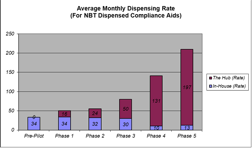
Figure 7. Average Monthly Workload NBT
We decreased patient waits by 50 percent
Phase 1
· Turnaround time: 22-46 hours
Phase 5
· Turnaround time: 21-26 hours
· (4.5 hours for “Golden Patients”)
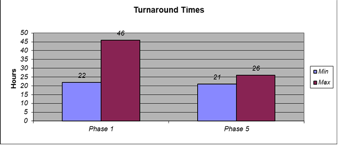
Figure 8. Average Turnaround: Phase 1 and 5: Hub
For our efforts to improve the use of compliance aids and promote safety in medicine use, we have been shortlisted finalists for several awards, including: finalists for the Health Service Journal (HSJ) Awards 2014; Finalists for the HSJ Value in Healthcare Awards 2014; Finalists for the Alliance Healthcare Pharmacy Awards 2011.
Conclusion
NBT has developed an innovative and mutually beneficial partnership between an Acute Trust and a commercial pharmacy provider to deliver a high quality patient-focused service for our patients, particularly for patients with long-term conditions, resulting in the successful management of increasing demand for compliance aids.
This has enabled:
- Faster turnaround of patients;
- Reduction in bed-blocking;
- Improved service for patients;
- Managing increasing workload demands.
In pharmacy, the implications are:
- Leaner processes and reduced workload in the dispensary;
- Improved skill mix in the whole process;
- Improved staff morale, reflecting smoother operational processes and reduction in complaints.
The increasing demand for compliance aids is an issue for Trusts nationally, and we feel strongly that our successful outsourcing initiative can be used in other Acute Trusts to improve practice and effectively manage the increasing demand for compliance aids in accordance with QIPP.
Future Work
We are now looking at:
- 7 days a week service
In Everyone Counts: Planning for Patients 2013/14, Sir Bruce Keogh, National Medical Director of NHS England highlighted seven-day services across the NHS over the next three years (NHS England 2013).
The new 7-day working approach is being adopted by NBT and the Hub is reviewing provision of a Sunday/ Bank holiday service.
- Further skill mix
In house, we are now looking at using band 3 technicians with the band 4 technicians.
- Re-launch of Pan Bristol
Assessment tool
We will also be liaising across Bristol and North Somerset to review and re-launch our assessment tool currently referenced on the RPS website.
Acknowledgements
We acknowledge NBT team members Andrew Davies, Director of Pharmacy; Val Giltrow-Tyler, Senior Pharmacist (IT), Jan Kenington, Senior Technician (Procurement Lead), Pharmacy Invoicing Team; Pharmacy Procurement, Pharmacy Home Care Delivery and Pharmacy Compliance Team (Band 3s, 4s + 5s) Lloyds Hub Team (Mike Hon, Hub Manager, LloydsPharmacy); AAH Pharmaceuticals Ltd and Celesio Hub Support Teams and Senior Leads: Andrew Morris, Head of Hospitals, AAH and Andrew Davies, Director of Pharmacy, NBT.
References:
Disability Discrimination Act 2005 (c.13). London: The Stationery Office.
Equality Act (DEA) 2010. (c.15). London: The Stationery Office.
Mahtani KR, Heneghan CJ, Glasziou PP et al. (2011) Reminder packaging for improving adherence to self-administered long-term medications. Cochrane Database Syst Rev, 9: CD005025.
National Institute for Health and Clinical Excellence (2009)
Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence. Manchester: National Institute for Health and Clinical Excellence. [Accessed: 18 February 2015] Available from https://www.nice.org.uk/guidance/cg76
National Patient Safety Agency (2007) Safety in doses: improving the use of medicines in the NHS. London: National Patient Safety Agency. [Accessed: 18 February 2015] Available from http://www.nrls.npsa.nhs.uk/resources/?entryid45=61625
National Patient Safety Agency (2009) Safety in doses: improving the use of medicines in the NHS: learning from national reporting 2007. London: National Patient Safety Agency.[Accessed: 18 February 2015] Available from http://www.nrls.npsa.nhs.uk/resources/?entryid45=61625
NHS England (2013) Everyone counts: planning for Patients 2013/14 to 2018/19 [Accessed: 18 February 2015] Available from http://www.england.nhs.uk/wp-content/uploads/2013/12/5yr-strat-plann-guid-wa.pdf
NHS England (2014) Risks arising from breakdown and failure to act on communication during handover at the time of discharge from secondary care. Patient safety alert, 29 August [Accessed: 18 February 2014] Available from http://www.england.nhs.uk/wp-content/uploads/2014/08/psa-imp-saf-of-discharge.pdf
NHS Institute for Innovation and Improvement (2008) Quality and service improvement tools. [Accessed: 18 February 2015] Available from http://www.institute.nhs.uk/index.php?option=com_quality_and_service_improvement_tools&Itemid=551.html
Picton C, Wright H(2013) Medicines optimisation: helping patients to make the most of medicines: good practice guidance for healthcare professionals in England. London: Royal Pharmaceutical Society. [Accessed: 18 February 2015] Available from http://www.rpharms.com/promoting-pharmacy-pdfs/helping-patients-make-the-most-of-their-medicines.pdf
Royal Pharmaceutical Society (2013) Improving patient outcomes: The better use of multi-compartment compliance aids. London: Royal Pharmaceutical Society. [Accessed: 17 February 2015] Available from http://www.rpharms.com/support-pdfs/rps-mca-july-2013.pdf



