HealthManagement, Volume 21 - Issue 3, 2021
Digital mental health services hold great potential for the future of mental healthcare provision; embedding the services in a stepped care model (with steps providing prevention or treatment of different intensities depending on the severity of the illness) and in a hybrid approach (integrating both virtual and in-person care) ensures that the services are accessible, flexible and adaptable.
Key Points
- Digital mental healthcare has the potential to bring more access, flexibility and cross-sectoral collaboration into mental healthcare provision.
- Digital services constitute a vital part of managing the COVID-19 crisis in the mental health services of the Region of Southern Denmark.
- On top of important aspects such as data security and privacy, coming challenges lie in ensuring health equality and minimising the digital divide.
- Ways forward for digital mental health lie in service formats independent of time, known as ‘asynchronous’, which can be combined with in-person encounters to a stepped and hybrid care concept across the entire mental health pathway.
Digital Technologies Have the Potential to Transform Mental Healthcare
Globally, there is a troubling increase in mental health disorders – a challenge further reinforced during the COVID-19 crisis. At the same time, a worryingly large proportion of people who experience mental illnesses do not seek the help or support they need, which widens the treatment gap. These unfortunate developments put pressure on our healthcare systems, while leading to a shorter life expectancy in the patient group, often from underdiagnosed comorbidities.
To counter these challenges, our mental healthcare systems are in need of transformation. At the Centre for Telepsychiatry in the Region of Southern Denmark, we believe these changes need to be interlinked directly with an increased use of digital treatment and support. Digital technologies have the potential to transform mental healthcare by connecting patients, services, and health data in new ways. They can make it easier and more convenient for patients to access mental health services and they offer flexibility in how treatment pathways can be personalised and adapted to individual needs and preferences. Benefits include shorter waiting times, avoidance of service gaps, and the potential cost-effectiveness of digital services.
Digital services can increase capacity of the mental healthcare system by allowing healthcare professionals to treat more patients. Asynchronous digital mental health services such as online therapy, digital monitoring of symptoms and social functioning, and self-care tools enabling people to take control of their mental health allow for promoting mental health and preventing mental illness.
Over the past decade, the use of digital health services has made it possible to reach patients in remote areas or with limited mobility so that they receive the treatment or monitoring needed. In this respect, the mental health field is no different from physical healthcare. But, as the field of digital mental health has grown and more services have been developed, tested and implemented, it has become clear that some people experiencing mental health problems benefit even more from digital treatment options than they would from in-person care.
Examples show that both travelling to see a therapist and keeping contact with a hospital can be stressful. People affected by anxiety or post-traumatic stress disorder can find the concept of travelling to see a therapist in person (and spending time in a waiting room) so demanding that they either give up entirely or are so exhausted when they get there that they are not able to fully benefit from the therapy offered to them. Staying in contact with a hospital can be challenging too. Some patients can find it crucial to get support by staying in digital contact with a hospital after discharge, or having digital contact with peers, which can help them transition back to life at home and avoid a readmission.
A particular challenge in the healthcare domain is the gap between mental and physical healthcare services. This is an important issue in the lives of people experiencing mental health problems. Many patients have comorbidities, which, if left untreated or treated in parallel and without coordination, can have serious consequences for the patients’ illness trajectory and quality of life. The use of digital technologies offers opportunities for increasing coordination across health and social care domains and for minimising any gaps on the patient journey. Digital technologies can be based on shared data that follows the patient, and they can even just make possible increased communication and coordination.
Building the right technology platforms and tools, which add value for both patients and healthcare professionals and systems, is crucial and requires close collaboration between everyone involved. Additionally, we need to invest in training, guidance and support to ensure that digital mental healthcare will continue to improve everyday care, even after the immediate threat of COVID-19 lessens.
Of course, however, digital technology is not a panacea for all our problems nor a replacement for in-person care. But digital therapy and support can and will offer increased access to treatment and improve outcomes for people with mental health problems. In the Centre for Telepsychiatry, we know this from experience, as we have spent many of the last years committed to the development, research and implementation of innovative technology-based interventions that are clinically relevant, safe to use and meaningful to our users in the Danish mental health services.
How Digital Mental Healthcare Has Proved Its Worth in the Midst of a Global Pandemic
In the Region of Southern Denmark, the development, validation and implementation of digital mental health services have been priorities for nearly a decade. The services range from well-known and well-tested technologies such as video consultations and internet-based Cognitive Behavioural Therapy (iCBT), to more cutting-edge innovations like Virtual Reality and Artificial Intelligence. Let’s look, first, at video consultations and after that, at iCBT.
As the pandemic hit in early 2020, digital services became an urgent need in Southern Denmark, and our experience with digital technologies enabled us to move fast. The most important task became to provide people with access to treatment and services, without compromising the health and safety of either patients or healthcare professionals.
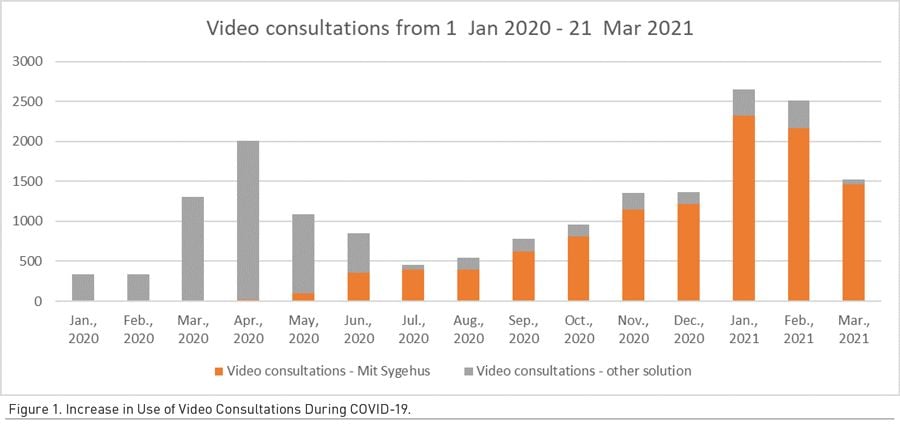
In our region, we immediately saw a dramatic increase in the use of video consultations (Figure 1). The service proved vital in managing the crisis in our mental health services. Within days, all outpatient care shifted to virtual visits, and 70% of consultations took place via phone or video. In the first week of the pandemic, we moved to a completely new video platform, ‘Mit Sygehus’ (‘My Hospital’) to meet the intense rise in demand (Centre for Telepsychiatry 2020). Key learning points from this experience taught us to focus on three critical issues: the importance of technical support and training, the establishment of local infrastructures of key contact persons to enable professional peer support, and the tailoring of support to both patients and staff.
With or without COVID-19, video consultations have several uses. They are used as a supplement to regular care, and for medication management, psychotherapy and other forms of support.
In Denmark, the video consultations service model has been implemented at scale since 2015 with reimbursement now equalling in-person consultations.
Another vital access point open to our patients was the online therapy clinic delivering iCBT for depression and anxiety. With this service, patients have access to online materials based on Cognitive Behavioural Therapy (CBT) self-help manuals designed to offer the same information as provided in regular CBT therapy. Over the past six years, our clinic has provided online psychological assessments, therapy and referral services to more than 4,500 patients. The online and largely asynchronous format ensures that patients have flexible access to therapy and support, while fostering self-efficacy in those patients who complete the programme. The service builds on a solid evidence base showing significant effect sizes comparable to face-to-face treatment, and with an average of 15-20 minutes spent with a patient per week, we see a reduction in the time therapists spend treating each patient compared to regular care.
The online clinic is a national digital mental health service funded by the five Danish regions in collaboration. It has been running as routine care since 2015. During the 2020 pandemic, permanent funding was secured for the service due to strong Danish policy support for online therapy services.
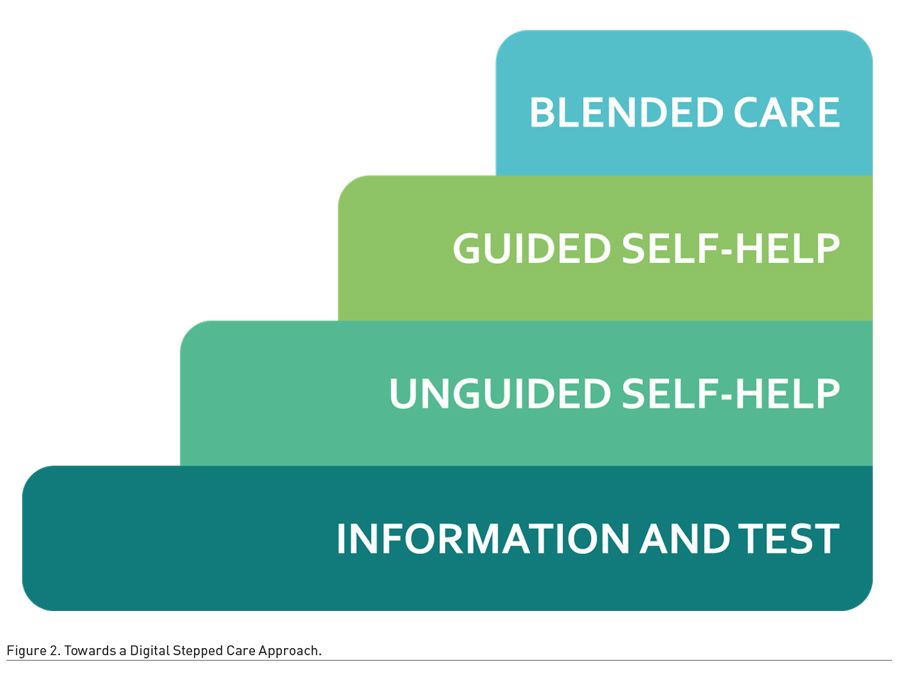
The clinic will form the basis for important development work in the coming years. The aim is to expand the range of treatment options (e.g. targeting new diagnoses) and work towards an unguided version of the therapy programme, which will allow for patients to access and complete the programme independently from psychologist support. It will also form part of a hybrid (or ‘blended’) care concept as the very top step of a stepped care model.
Digital care works well if it is introduced through a series of steps or stages. In the Centre for Telepsychiatry, we are working towards a digital stepped care approach, as illustrated in Figure 2. The model will consist of a number of distinct steps that move from stand-alone to guided forms of care, where virtual and in-person care formats are blended into a hybrid format. Depending on the severity of the patient’s illness, we can provide steps that range from basic information over asynchronous and unguided treatment to synchronous real-time treatment blending virtual and in-person consultations.
Making Digital Transformations Stick
Digital transformation has started, but basic questions remain about how it will stay – in 2021 and onwards.
All over Europe, conversations related to digital health were influenced deeply by a shift in needs caused by the 2020 pandemic. The discussion at the 2020 EHTEL symposium was no exception. Digital mental health featured in the programme with the session ‘Contributing to improved health and community resilience: the role of eMental health’, including contributions from the Centre for Telepsychiatry and GAMIAN Europe. The session has since spun out into a new workstream, which the Association is promoting, that focuses on hybrid care (Box1). Among other initiatives, it will materialise in a series of webinars in 2021.
Box 1. Hybrid care can be described as a merging or bringing together of both physical encounters (e.g., appointments or health visits) and virtual encounters between health and care professionals and patients in the same treatment pathway.
At the Centre for Telepsychiatry, our focus now is to learn from the extraordinary circumstances brought on by the pandemic in 2020 and keep our momentum on sustaining digital mental health services. The digital format may not continue to function at the same pace and scale in 2021 and beyond. However, in a post-pandemic setting, we believe strongly in the flexibility of combining treatment formats in a hybrid care concept, as part of a stepped care model. The approach will enable us to provide the appropriate level of care and support for each patient.
There are many benefits to digital mental healthcare. The treatment format shows increased flexibility and potential cost-effectiveness. In the centre, we have a strong evidence-base for how digital mental health can be used to offer effective care in several psychiatric conditions, when combined with regular care. For instance, smartphone apps can be useful tools for some patients, but their effectiveness more than doubles when they are used with some form of human support, e.g. in collaboration with a healthcare professional.
We anticipate that using digital therapies in the mental health field is more than likely to stay with us.
Moving Forward with Digital Mental Health
The 2020 pandemic has changed mindsets and paved the way for virtual care all over the world. And even though the sustainability of this transformation has not yet been evidenced, we do see a greater acceptance of the digital format in physical as well as mental healthcare.
The benefits of digital mental health are profound, but can only be achieved if digital tools are trusted and used by both patients and clinicians. For this to stick, we need data-safe and user-friendly digital solutions targeting unmet needs, training of healthcare professionals, clinical guidance around implementation and delivery, as well as patient partnerships in digital service design.
Despite the many and well-known benefits of digital mental health, concerns prevail about data security and privacy, the digital divide, health inequalities and the uneven evidence-base for effectiveness. In the Centre for Telepsychiatry, we strive to ensure that our services are both safe and effective – efforts supported by our in-house research unit and data management team. A bigger challenge is tackling the digital divide, which seems to increase with the growing use of digital services.
Certain patient and population groups risk are being left behind if they do not have access to digital services. Accessibility depends on the availability of technological equipment, a solid internet connection and the digital skills needed to use the services. So, on top of building the right digital health solutions and platforms in collaboration with the relevant users, we also have to focus on how to make these equally accessible and inclusive for all. For this reason, we are focusing our efforts on developing digital skills in both healthcare professionals and patients to prepare for a sustained use of digital solutions after the end of the pandemic.
To conclude: Mental health affects us all. There is no doubt that digital mental healthcare can make a valuable contribution to improving the lives of people who are experiencing mental illness, and in turn the people around them. For the digital mental health field to reach significant scale, however, we see the future of mental healthcare to lie in its freedom from time constraints: it can serve patients at any time of the day or night, as needed, and healthcare providers can adopt a one-to-many approach thus avoiding additional strain on healthcare systems. Used in meaningful combination with regular care, this is where digital technologies can really move mountains.
Conflict of Interest
None. 
Centre for Telepsychiatry, Region of Southern Denmark
The Centre for Telepsychiatry is an innovation and research centre within the Mental Health Services in the Region of Southern Denmark. The centre aims to increase access to mental healthcare and improve health outcomes for people with mental health problems by co-designing and delivering digital interventions on regional, national and international levels.
EHTEL – the European eHealth stakeholder platform
EHTEL (the European Health Telematics Association) is a unique pan-European multidisciplinary stakeholder organisation, which brings together corporate, institutional and individual actors dedicated to the improvement of healthcare delivery through digital health. Recently, EHTEL has been strengthening its efforts in digital mental health as a focus area in its hybrid care workstream.
References:
Centre for Telepsychiatry (2020) Video consultations in mental health: Swift implementation during COVID-19. EHTEL. Published 28 August. Available from iii.hm/18kh





