HealthManagement, Volume 21 - Issue 2, 2021
Faced with the necessity to share information from the electronic patient record across different systems, a regional hospital in Belgium introduced a disruptive ‘only once’ approach to deploy a SNOMED CT coded patient summary and minimise the relevant burden on the clinical staff.
Key Points
- The information from the electronic patient record has to be reused in different contexts, which requires excessive copying and burdens the clinicians.
- To address this time-consuming challenge, the ‘only once’ approach was introduced.
- Based on the SNOMED CT codes, the use of diagnosis codes had significantly increased within the first year of implementation.
- There are several success factors, including the ease of use and increased time efficiency.
CHR Haute Senne is a regional hospital of 246 beds with 8,400 in-patients per year, 7,100 daily hospitalisations, 180,000 consultations and 26,500 emergency visits. 150 physicians fill out an integrated electronic patient record (EPR) on a daily basis. Each medical speciality customises their own sections and fields in this medical file. The main advantage of this software is that each contact with the patient is online, documented by the clinician, which promotes the continuity of care.
However, at some point it became apparent that some key information such as diagnostics, procedures and medications, needed to be reused in different contexts. This led to unnecessary copying, which is a source of errors. For example, the admission diagnosis must be transmitted from the emergency department to the downstream hospitalisation unit, the public paying agency, the national register of emergency department visits and medical coding.
To meet this challenge, in 2017, we proposed to the physicians two alternatives:
1) We retain a classic data-driven approach by not changing anything in the EPR, but by requiring the same re-encoding in all applications where diagnostics is needed.
2) We ask for a minimal effort from the doctor (3 clicks and 30 seconds) including highlighting the relevant diagnoses, pressing a keyboard key (F10) and selecting the coded diagnosis(es) to be fed into a Patient Summary.
Our emergency physicians and ward physicians quickly did the math: it was the second option that was both the fastest and the most productive with its ‘only once’ approach.
Technical Characteristics
We named this project RCMax (“Résumé Clinique Maximum” in French).
The chosen coding system is SNOMED CT (Systematized NOmenclature of MEDicine – Clinical Terms). SNOMED CT has been defined as the most comprehensive medical terminology and allows a consistent representation of the clinical content of electronic health records. It is a terminology close to the common clinical language and is intended to accurately match the information provided by the clinician. It is an input-based system structuring the data entry.
The software called ‘Snomedizer’ displays a list of SNOMED CT-coded diagnostic candidates extracted from a terminology server based on a free-text entry highlighted by the physician.
We have set the goal of having at least one SNOMED CT-coded verified admission diagnosis per hospitalisation. After a pilot year in 2017, with a dictionary limited to 6,000 diagnosis codes, we proposed a much wider range of 170,000 entries in French, covering a large majority of the pathologies encountered. If certain diagnoses are not found, we have the possibility to locally enrich the terminology server with, in particular, the use of synonyms applied in common clinical language that point to the official SNOMED CT preferred terms. In 2018, 25,000 diagnoses were recorded by physicians in the patient summary, with approximately three codes per hospitalisation.
It should be noted that this Patient Summary follows the patient in their clinical history, with links to the documents behind the coded choice of the physician, for example, a hospitalisation report.
This makes it possible to return at any time to the authentic source detailed in free text. On the other hand, the system manages the start and end dates dynamically, which allows to automate the notion of antecedents: an antecedent is a diagnosis that has an end date in the past, which makes it inactive and therefore filed by the programme in a separate section. In addition, the context data can be modulated: degree of certainty, laterality, notion of family antecedent. By default, to be quick, the chosen diagnosis is supposed to be confirmed, there is no laterality, and it concerns the patient and not their family.
The system has enabled the systematic display of the Patient Summary when a file is opened, which immediately informs the clinician of the patient’s active diagnoses. The reuse of codes has automated the sending of the admission diagnosis to the public paying agency and to the various disease registries involved. But where the added value was the most dramatic, was that we reused the diagnoses in SNOMED CT to automatically convert them via an international mapping table into ICD10 codes, used for the management of funded length of stay (LOS). Indeed, since 2020, in real time, the hospitalisation unit physician can see the pathology profile (DRG: Diagnosis Related Group) to which a national average LOS corresponds, as soon as the main diagnosis and possible co-morbidities are encoded. The coding thus provides a bridge between the clinical documentation of the Patient Summary and the management of the LOS, which serves as a basis for funding. This is all the more strategic since almost half of the hospital’s (and thus, indirectly, the physicians’) income comes from the financing of the pathology profiles (DRGs) of hospital stays.
Success Factors
The success of the deployment of this online coding system can therefore be explained by four factors:
1. Clearer EPR through the shared medical management of a Patient Summary common to all physicians.
2. It saves time for the clinician who does not have to re-encode the diagnoses in different applications (‘only once’).
3. Ease of use (3 clicks in 30 seconds)
4. Online management of the financed stay.
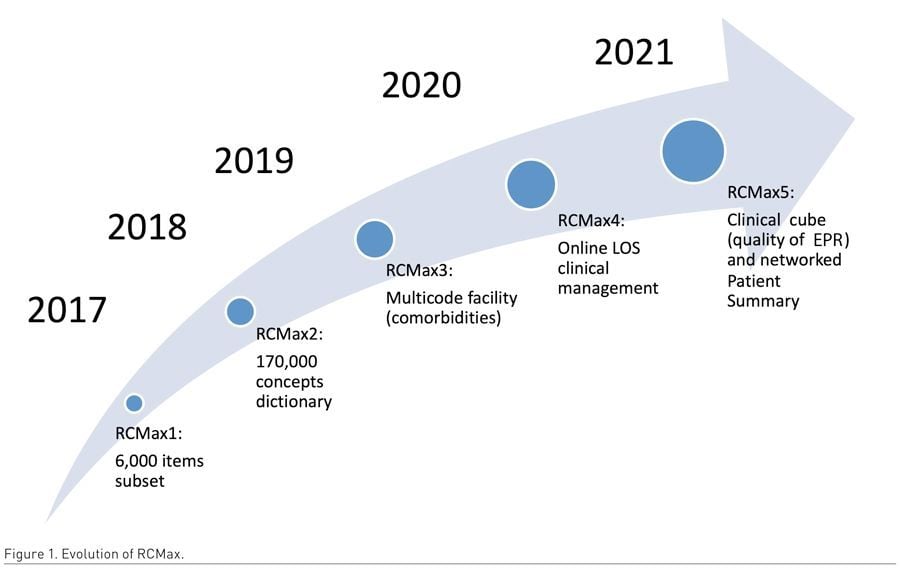
The road travelled by the RCMax project is already long, but there are still steps to be taken (see Figure 1). The first one is the extraction of data for strategic management purposes (quality of the Patient Summary, LOS management) via a clinical cube in the data warehouse. The second step is the harmonisation of the hospital’s Patient Summary with that of the first line of GPs (General Practitioners) via Health Networks.
In conclusion, the implementation of a SNOMED CT-encoded Patient Summary has allowed, through a disruptive ‘only once’ approach, to change the encoding of diagnoses in a Patient Summary in favour of continuity of care; an overall time saving through the reuse of encoded diagnoses; and a medical optimisation of stays towards better quality and justified financing.
Conflict of Interest
None. 



