HealthManagement, Volume 21 - Issue 1, 2021
Key Points
- Gioia Foundation is the charitable institution involved in the project.
- The goal of the project was to identify a support technology that could help first-line healthcare personnel in the critical wards where severely ill COVID-19 patients were treated.
- The aim of the project was to donate a high-end ultrasound system for diagnosis and follow-up of COVID-19 patients, reducing the need to move patients to the dedicated radiology unit.
- The Center for Instrumentation Sharing of the University of Pisa was selected for deployment in the ICU for immediate relief during the COVID-19 emergency as well as for reuse in other research applications.
- The installation of the ultrasound system in a clinical environment with research experience allowed to obtain measurable benefits not only in patient care but also in the production of scientific results.
Pisa is a small Italian town of 90,000 inhabitants. It is world-renowned for its iconic leaning tower and for being the birthplace of Galileo Galilei, who taught at the local University and is considered the father of modern science. In recent times, the University of Pisa had two Italian presidents, five Italian prime ministers and three Nobel Laureates as students, faculty or staff affiliates.
Moreover, Pisa has a tradition as a leading Italian industrial site for pharmaceutical production, is in the forefront of gravitational waves research (one of the three interferometers in the world is located in Pisa), is the only Italian centre having a 7T MRI system operational since 2012, and has an outstanding reputation in transplant and robotic surgery.
In this unique historic cultural environment several charitable institutions were established in recent years. During the COVID-19 pandemic, they played a significant role in helping local health authorities cope with the emergency situation.
Most charitable initiatives were aimed at addressing the initial shortage of personal protective equipment (PPE), and at mitigating the suffering of gravely ill intensive care unit (ICU) patients that were unable to communicate with their loved ones. For the latter initiative, dedicated Wi-Fi networks were put in place and tablets were given to patients in order to enable them to be in touch with family members who were not allowed in the hospital for a visit (https://fondazionearpa.it/a-wifi-rainbow-over-the-hospital-walls/).
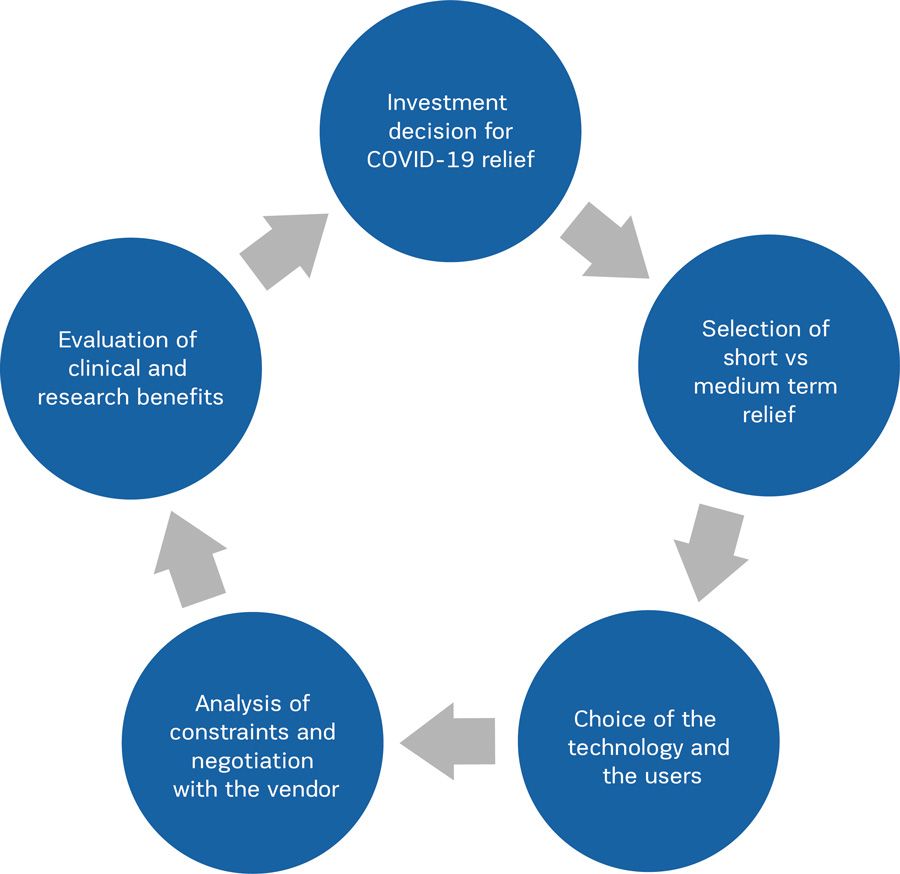
A different type of charitable initiative led to the purchase of a high-end ultrasound (US) system for the ICU physicians. In this paper we will briefly describe how this project was speedily envisioned and implemented and what were the lessons learned (Figure 1).
The Project
The charitable institution (Gioia Foundation) involved in the project is headed by Maurizio Mian, the last scion of a family counting some university professors in different medical disciplines and having a fruitful osmosis with a pharmaceutical company (Istituto Gentili) and its research division, whose director, Sergio Rosini, was responsible for the outstanding discovery of one molecule active in the treatment of osteoporosis.
The Gioia Foundation proposes itself as the ideal extension of the research activity of these prestigious forerunners and invests in charitable projects in the Pisa area.
When the pandemic started to rage in spring 2020, most investments and donations were aimed at mitigating immediate problems linked to the overflow of patients arriving to the hospital in severe conditions. On the contrary, the Gioia Foundation project was envisioned with the aim to answer a more strategic question: “Which support technology could make a difference in this healthcare crisis?” Such an approach was uncommon in the early days of the pandemic, and its merit was to analyse the new workflows forced by COVID-19 and to identify a support technology that could be of help to the first-line healthcare personnel in the critical wards where severely ill COVID-19 patients were treated.
Which Technology?
The Pisa University hospital is spread over several buildings. During the initial months of the pandemic, one of the challenges was to move COVID-19 patients safely from some of these buildings to the Radiodiagnostica 1, which was the radiology unit dedicated to serve the highly contagious COVID-19 patients. In this context, it was noticed that one of the main ICU was staffed by superbly trained intensivists with good experience in the use of bedside US systems for the ultrasonographic evaluation of the lungs. The aim of the project was to donate to these first-line physicians a high-end US system able to assist them in the diagnosis and follow-up of COVID-19 patients, thus reducing the need to move patients to the dedicated radiology unit. In fact, pulmonary US was reported being able to document involvement of COVID-19 by demonstrating signs suggestive of interstitial-alveolar damage and by showing diffuse pleural line abnormalities, sub pleural consolidations, white lung areas and thick, irregular vertical artefacts (Buonsenso et al. 2020).
Which Vendor?
Once the technology was selected, the next issue was to assess which vendor was able to expeditiously deliver an US system with all the technical features needed for the required application, and possibly with a sufficiently complete set of functionalities to grant other advanced applications after the end of the COVID-19 emergency. Finally, price and delivery time were taken into consideration.
Several vendors were contacted and their offers were compared by using a quantitative method. The final choice was a US system meeting the high-end quality requirements for performing US examinations of the lung while retaining the potential for being re-used after the pandemic in research involving other clinical domains.
The instrument was directly purchased by the project in order to maximise the effectiveness of the negotiation. In fact, the project was able to obtain nearly 65% discount on the original price (60,000 Euro instead of 168,900 Euro, VAT excluded) and a delivery time of less than two weeks: the order was issued on March 27, and the installation of the US system took place on April 10, 2020.
Which User?
The choice where to install the new equipment was guided by the following requirements: presence of clinical experience of US examinations performed on critically ill patients and multidisciplinary integration of medical and technological competence. This led to the selection of the Unit of Anesthesia and Reanimation that had the experience needed to study the acute respiratory insufficiency US patterns due to SARS-COv-2 infection and to compare them to other pulmonary US patterns due to pulmonary oedema, cardiac insufficiency and sepsis-induced ARDS. This is particularly important since the US diagnosis based on the operators’ visual analysis of the images can be implemented with an algorithmic analysis that has the potential to lead to early identification of SARS Cov-2 patients and to quantify the changes in lung involvement during follow-up.
Which Institution?
The main issue was to choose whether to donate the US system to the hospital or to the University. Two factors were taken into consideration: the regulatory constraints of the beneficiary institution and the flexibility in the deployment for allowing a possible reuse after the end of the pandemic. On the basis of such analysis, the Center for Instrumentation Sharing of the University of Pisa (CISUP) was selected because it guaranteed the immediate deployment in the ICU for immediate relief during the COVID-19 emergency as well as for later reuse in other research applications (https://www.facebook.com/CISUPofficial).
Lessons learned
Our experience shows that in an emergency situation, a strategic vision may help to address needs that are not apparent if only the immediate relief is taken into consideration. The ample degree of freedom granted to a charitable organisation helped to “think outside the box” and to overcome the constraints of a highly regulated environment such as the Italian one that usually prevents speedy relief investments. The installation of the US system in a clinical environment with research experience allowed to obtain measurable benefits not only in patient care but also in the production of scientific results. Indeed, two scientific papers were written in the months immediately following the donation describing novel clinical applications made possible by the donated US system (Corradi et al. 2020a; Corradi et al. 2020b).
Conflict of Interest
None.
References:
Buonsenso D, Piano A, Raffaelli F, Bonadia N et al. (2020) Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci., 24(5):2776-2780. doi: 10.26355/eurrev_202003_20549.
Corradi F, Vetrugno L, Orso D et al. (2020) Diaphragmatic thickening fraction as a potential predictor of response to continuous positive airway pressure ventilation in Covid-19 pneumonia: A single-center pilot study. Respir Physiol Neurobiol., 284:103585. doi: 10.1016/j.resp.2020.103585.
Corradi F, Isirdi A, Brusasco C et al. (2020b) Low diaphragm muscle mass predicts adverse outcome in patients hospitalized for COVID-19 pneumonia: an exploratory pilot study. Minerva Anestesiol-15129. Accepted for publication




