HealthManagement, Volume 19 - Issue 4, 2019
Summary: It is estimated that even today, medical errors are the third leading cause of deaths in the US, costing the health system several billions of dollars a year. Many of these deaths can be attributed to the misuse of medication.
When used properly, medications save lives. Unfortunately, medication and dosing errors are one of the top challenges that hospitals face and can lead to patient harm and even death. Hospitals implemented electronic infusion pumps in the 1970’s to provide more precise flow control of fluids, medications and nutrients than manual adjustment of gravity infusions alone could provide. But along with these benefits to patients came pump-related errors in the tens of thousands. Indeed, the prestigious ECRI Institute’s “Top Ten Health Technology Hazards” list has included infusion pumps in eight out of the past ten years, including 2019, and in 2010, the US FDA changed guidance about infusion pump design, based on five years of adverse events and recalls reported to the FDA by hospitals and manufacturers.
You might also like:New hospital polices and procedures required for patient safety
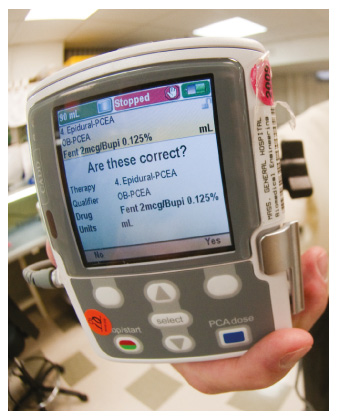
In 1985, a multidisciplinary team at Massachusetts General Hospital, motivated by a near-miss event involving a life-critical infusion in a newborn, started working on creating better, more portable drug infusion pumps, using recent advances in low power microprocessors and other technical advances permitting equipment miniaturisation. Our first device was a small syringe infusion pump that assisted users in making complex dose calculations. Subsequently, we developed, patented, and then widely licensed to industry the concept for “smart drug infusion pumps.” These allow a hospital to embed in the pump’s user interface a table, called a “drug library,” of their own, customised list of drugs, together with the best practices by which they are given. The pumps had the capability to prompt a user for correct practices, and to detect and prevent programming errors before they reached the patient. In 2002, ECRI Institute named this feature a “Dose Error Reduction System.”

The advent of “smart pumps” and other patient safety technologies, such as bar-code-assisted-medication-administration (BCMA) prompted leading healthcare systems to launch ambitious initiatives to achieve continuous excellence, and to target “Zero Medication Errors” as achievable goals. In 2005, Partners Healthcare System, in Boston, Massachusetts, where I work, set a goal of reducing medication errors through technology by 2010. We implemented multiple technological systems and changes to the workflow of front-line caregivers and support staff. These included computerised order entry with decision support and the development of our own electronic medication administration record system with bar coding. We worked with our insurers and payers to mandate and implement smart drug infusion pumps at every patient bedside. By 2010, modern versions of “smart pumps” were wireless-capable, permitting drug libraries to be updated more frequently. However, the full electronic integration of the pumps with our clinical information systems, for example with patient-specific order entry, the pharmacy information systems, and the care documentation systems, could not actually be completed by the target date of 2010, for a host of reasons including cybersecurity, the sophistication of wireless information networks, lack of harmonisation of the drug libraries with the formulary, and the sophistication of the pump programming screens.
In 2014, Bill Churchill, Pharmacy Director at Brigham and Women’s Hospital, and I proposed a new timeline for “pump integration” in our Boston hospitals, at the World Patient Safety, Science & Technology Summit. The revised goal was to have a system in place by the year 2018 that could exchange data in real-time between pumps and clinical information systems, while providing auto-programming and auto-documentation. In January of 2019, we affirmed this timeline with the Patient Safety Movement Foundation, because our organisation had made a system wide decision to implement one single infusion pump platform across all 13 of our hospitals … to fully integrate clinical systems to minimise medication errors and close the loop with intravenous drug pumps.

As I write this in the late spring of 2019, it is the “go-live” date for implementation of the new, closed-loop-capable pump platform, at the second largest of the 13 hospitals at Partners Healthcare System (Brigham and Women’s - BWH). 3,800 infusion pumps are being replaced in one day, with large teams of support staff in constant attendance to ensure patient safety and continuity of care at the transition moment. All the team members have special T-Shirts with the hospital logo and “Pump Go Live Team – Leading Innovation!!” The Hospital’s public-facing newsletter makes it clear that “failure is not an option” even if glitches arise, as is inevitable: “The transition is part of a system-wide goal of wireless, auto-pump programming and auto-documentation in Partners ‘eCare’” (bwhbulletin.org/2019/05/23/get-pumped-brigham-completes-infusion-pump-transition). After BWH is settled, the other 12 hospitals will follow in a pre-defined sequence. And at each hospital, the target features of “auto-programming” and “auto-documentation” will be achieved according to the implementation plan.
You might also like: Achieving zero avoidable patient deaths by 2020
In 1985, our team stepped out of our ‘day-job’ descriptions, to set aside time to design and to develop entirely new kinds of drug infusion pumps, effectively partnering with mainstream industry and with start-ups, too. We are proud of this effort, prompted by the incident with the newborn baby, and by the desire to have better technology with which to do the best possible patient care.
In 2005, Our Partners Healthcare System Leadership Wrote Defining a Pathway That Has Been Emulated Widely
“By 2010, most Partners hospitals will have fully integrated clinical systems to minimise medication errors. These integrated systems will allow physicians to order medications and tests electronically via a computerised order entry system. With “medication decision support” software integrated into Partners’ computerised order entry systems, physicians will be able to reconcile medications and identify possible adverse drug interactions and patient allergies electronically - before an order is placed. These systems will also enable nurses to electronically record medications administered to patients and ensure that the right patient gets the right drug at the right dose at the right time. By scanning their own bar-coded staff identification, the patient’s bar-coded identification, and the patient’s unit dose bar-coded medication into the electronic medication administration records (eMAR) system, nurses will verify the accuracy of the medication administered and document the transaction electronically. Similarly, if the medication is intravenous, “smart intravenous pumps” will document the administration of these drugs in the eMAR system” (partners.org).
In 2013 ECRI Wrote
“Another important consideration is to recognise the limits of safety technologies. Many pumps today are equipped with on-board drug libraries that trigger alert warnings for gross miss-programming. Such “smart” technologies do a good (not perfect) job of helping to get the dose correct. This requires, however, that appropriate drug libraries are developed (and maintained) and that staff use the available safeguards appropriately. In addition, these technologies don’t help prevent errors such as administering an order to the wrong patient or selecting the wrong drug. Infusion pump integration – that is, connecting the servers for the infusion pumps with other information systems – can provide additional protections, such as helping verify that both the right patient and the right drug have been selected. Thus, we recommend that healthcare facilities begin (or continue) to implement infusion pump integration with relevant information systems” (ecri.org/Resources/Whitepapers_and_reports/2014_Top_10_Hazards_Executive_Brief.pdf).
This Year ECRI Wrote
“Even “smart pumps” that incorporate a dose error reduction system can be misprogrammed in a way that could lead to patient harm. The surest way to eliminate manual-entry errors is to implement auto-programming of your infusion pumps” (ecri.org/Resources/Whitepapers_and_reports/Haz_19.pdf).
It was a long road to this point, but I truly believe we have had, and by our leadership will continue to have, the opportunity to significantly reduce harm and death from medication errors around the world.
There is certainly more to be done. We will continue to find, fund, and facilitate pilot projects (particularly in oncology, anaesthesia, and critical care) that permit rigorous testing, verification, validation, and user acceptance of such integration, prioritised according to their impact on patient safety and capability of being scaled across the U.S. and global healthcare landscape. Of importance is continuing to refine the use of bar coding or other automatic identification technologies to assure automatic drug identification by drug infusion systems in every care setting. We also seek to assure that adequate online, highly scalable training and education technologies are available to all caregivers as they learn to use these advanced technologies. And we envision a future state in which human physiology, such as the depth of anaesthesia, can be precisely adjusted by drug infusion devices that are responsive to signals that measure each patient’s brain state in real time.
As Churchill said during World War II, “Now this is not the end. It is not even the beginning of the end. But it is, perhaps, the end of the beginning” (Winston Churchill 1942). This quote is applicable to our goal of ZERO preventable deaths from medication errors.
Key Points
- Medication and dosing errors can lead to patient deaths
- In 1992, a team at Massachusetts General created and licenced a “smart drug infusion pump”
- “Smart pumps” along with other safety technologies inspired “Zero Medication Errors” as goals
- The target date of 2010 could not be achieved because of a host of reasons
- A revised goal for 2018 was made to have a system that could exchange data in real-time between pumps and clinical information systems
- In January 2019, this timeline was shared with the Patient Safety Movement Foundation
- Spring 2019, the “go-live” date for implementation of the new, closed-loop-capable pump platform, took place
- 3,800 infusion pumps were replaced in one day
References:
Get-pumped-brigham-completes-infusion-pump-transition (2019) Available from Bwhbulletin.org/2019/05/23/get-pumped-brigham-completes-infusion-pump-transition/
Safety Technology Leadership invited presentation (2007) by the author; Annual National Patient Safety Foundation Patient Safety Congress, slides 4 and 5. Available from partners.org
Top 10 Health Technology Hazards for 2014 Health Devices. (2013) Available from ecri.org/Resources/Whitepapers_and_reports/2014_Top_10_Hazards_Executive_Brief.pdf
Top 10 Health Technology Hazards 2019. Executive Brief. A Report from Health Devices. Available from ecri.org/Resources/Whitepapers_and_reports/Haz_19.pdf



