Leadership comes first.
High-quality patient information is crucial to the success of personalised care. Leadership from the management team is critical in embedding patient information throughout patient pathways.
Why should healthcare managers make patient information a priority when there are so many other pressing items on the agenda? The answer is simple. Without access to high-quality, accessible health information the move to personalised care will fail. High-quality healthcare information, which is developed with its users, is the common foundation to the six pillars of personalised care identified by the National Health Service (NHS) England (2017):
- Shared decision-making
- Long-term conditions care and support planning
- Patient choice
- Social prescribing
- Patient activation
- Personal health budgets
Why healthcare information?
There is already overwhelming evidence that health information, when it’s reliable, clear and provided at the right time and right place for the individual, is hugely beneficial (Patient Information Forum 2013). And what’s more, a person’s right to information to inform their care is enshrined in the NHS Constitution (Department of Health and Social Care 2012).
But patients still report they are not receiving the information and support they need to make informed decisions about their health and wellbeing. In a survey by Patient Information Forum (PIF) of 1,500 people with long-term conditions (Duman et al. 2015), 36% said they did not have enough information when first diagnosed. This figure rose to 58% for 18-24 year olds. And in 2016, only 56% of hospital in-patients felt involved in decisions about their treatment (Care Quality Commission 2017).
Patients’ responsibilities and rights
As the NHS creaks under pressure, there is a renewed push for people to take greater responsibility for elements of their own care. But if we’re going to take responsibility for our health, then it’s essential our rights as patients are met. Putting patients in control through access to information and support will enable people to take greater responsibility. With a growing emphasis on shared decision making (National Institute for Health and Care Excellence 2017), the first step needs to be ensuring everyone can access basic information, whatever their level of health literacy. And it’s worth bearing in mind that up to 61% of working age adults lack the literacy and numeracy skills to understand health and wellbeing information as currently produced (Coulter and Collins 2011).
What needs to change?
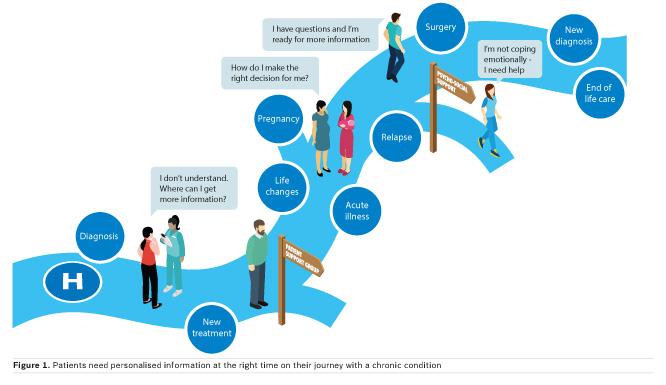
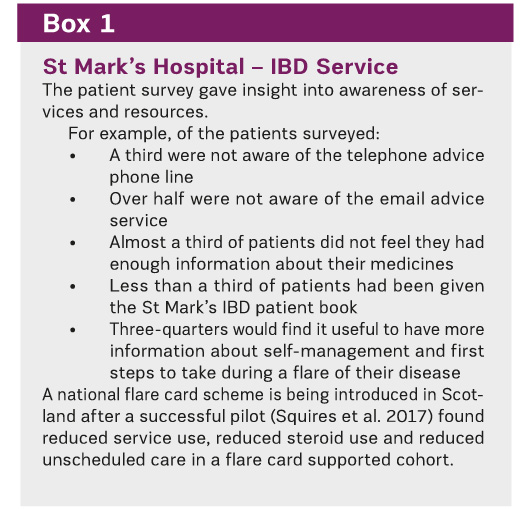
The good news is that high-quality information, and the tools and resources to support shared decision-making and self-management already exist and are being developed further. The problem is they are often not made widely available to patients (see Box 1 for results of the patient information survey we carried out at St Mark’s Hospital). To address this issue, the Patient Information Forum worked with patients and clinicians to identify and create a pathway that embeds the provision of accessible and tailored health information into the provision of care, from diagnosis, through treatment, to longer-term management (Figure 1).
The perfect patient information journey
Working with patients and clinicians, supported by AbbVie, the Patient Information Forum has developed a seven-step process to support healthcare services to develop and embed patient information across their pathways (see Figure 2). By using this process, services can create a ‘Perfect Patient Information Journey’ and transform the information experience of patients in a matter of months. By putting patient information needs at the forefront of service planning and by thinking about the Perfect Patient Information Journey for patients, healthcare professionals can ensure that individual patients receive the right information, in the right format, at the right time.
Leadership is critical
Leadership is essential to make sure everyone in a service knows their role regarding patient information, to make sure it is a priority and guarantee it happens. Ensuring that the leadership team of a service understands the value of information to patients is critical in changing the culture and embedding information throughout the pathway.
In busy, complex services, having clear roles and responsibilities amongst staff for information provision is crucial. Think about:
- Who will lead the seven-step process?
- Who can review available patient information sources from other sources and approve them?
- Who will be responsible for embedding patient information within care pathways?
- Who will make sure all staff know what is available?
Learning from pilots
The seven-step process was tested at two pilot sites; the inflammatory bowel disease (IBD) service at St Mark’s Hospital, North West London (a recognised centre of excellence) and Hereford Hospital Trust. Both pilots demonstrated the importance of investing time in the process and in having clear leadership to drive improvements across an organisation.
The IBD pilot study revealed a wide range of information needs through the process of gaining patient and staff insights, including a lack of awareness of patient support services designed to boost efficiency (see Box 1). The Hereford pilot showed that lack of appropriate information was a source of common complaint, particularly related to discharge (see Box 2).
PIF’s next step on the project is to develop and pilot a template for evaluating the impact of information interventions.
Ensure delivery of patient rights to information
PIF would like to see every healthcare service adopt our ‘Perfect Patient Information Journey’ and use the seven steps to embed and signpost high-quality, easy-to-understand and simple-to-access information for patients when they need it.
In failing to provide patients with all the information and support they need to participate in decisions about their healthcare, the health service is currently compromising all three key dimensions of quality care: patient experience, patient safety and clinical effectiveness. If patients are to take greater responsibility, we need to respect their rights and enable them to participate.
So, to the Government and others who are calling for patients to take greater responsibility for their health, we would challenge them to step up and meet their responsibilities to ensure that patient rights to information are met and delivered.
Key Points
- Patient information is a management issue, it can improve outcomes and reduce service use if people are empowered to self manage.
- Patient information underpins the six pillars of personalised care
- Patients report being uninformed about their care and only 56% of hospital in-patients felt involved in decisions about treatment
- Ensuring information is health literate makes services accessible and helps tackle inequality
- PIF has developed a 7-step process to deliver a perfect patient information journey
- If the NHS wants people to take more responsibility for their health it needs to provide or signpost information they can use and act upon
Conflict of interest
The Perfect Patient Information Journey project was funded by an educational grant from AbbVie.
PIF’s expertise in facilitating the development of a Perfect Patient Information Journey using the 7-step process is available on a cost-effective, not-for-profit consultancy basis to NHS Trusts and other bodies. For further information contact: Sophie Randall, Project and Partnership Manager
[email protected]
For more information on the Patient Information Forum visit www.pifonline.org.uk