HealthManagement, Volume 21 - Issue 7, 2021
Resources and costs associated with the treatment of chronic diseases account for more than 80% of total healthcare costs in many countries. As our population grows older and with more lifestyle issues and obesity among younger generations, the challenge of chronic diseases will increase in the coming years. New research documents that a new approach to chronic patients can significantly reduce resources and costs and at the same time improve patients’ quality of life and help them live longer with their disease.
Key Points
- Resources and costs associated with the treatment of chronic diseases account for more than 80% of total healthcare costs in many countries.
- The Epital Care Model (ECM), a research-based new treatment model, focuses on optimising the treatment of chronic patients.
- The ECM treatment model is more powerful than traditional telehealth because it is based on an optimised patient-centred approach and procedures.
- The 6 step ECM model incorporates clear thresholds and procedures which allow certain tasks to be transferred to non-clinical staff in a secure and regulatory compliant way.
- Technology alone does not lead to new models of care. There needs to be a re-design of the organisational setup which enables healthcare organisations to optimise the value which new technology can provide.
Chronic Patients and Our Current Healthcare System
If we go back in history to the 19th century when the first healthcare systems emerged, the background and driving force was a focus on acute care and the ability to help people who were injured in wars, accidents or who suffered from infections or infectious diseases.
Today, healthcare systems continue to carry reminders of past ways of organising themselves and the underlying culture that underpinned this, although the growing challenge of chronic diseases has radically changed both context and needs. Even though primary care is established and provides an increasing and important contribution to patient-centric healthcare, it is evident that today’s healthcare systems have not been designed with chronic patients in mind.
Chronic patients rely on compliance and on the ability to keep their chronic disease well-regulated and in perfect balance. The obvious example which everybody would understand is the diabetes patient who needs to constantly ensure that their insulin is balanced with their food intake. But the same need for constant compliance is also vital for other chronic patients – e.g., COPD and heart patients. If the period between the first symptoms of exacerbation or worsening and clinical intervention is too long, the result is often a faster deterioration over time of the patient’s health status. COPD patients who experience a higher number of severe exacerbations which result in hospital admittance lose their lung capacity faster than patients who are compliant, well-regulated and avoid severe exacerbations.
The Epital Care Model - A Healthcare System Designed for Chronic Patients
How do we design a healthcare system for chronic patients with a focus on their need for prevention and early intervention? One possible solution could be a reorganisation of services in a proactive direction using Patient Related Outcome Measures (PROM) data generated by patients through telehealth technology. This solution was tested out by a group of physicians, researchers, and municipalities in Denmark back in 2011 when they established the Epital Care project. The Epital Care project led to the Epital Care Model (ECM), a research-based new treatment model with a focus on optimising the treatment of chronic patients. The ECM model is not a completely new healthcare system as such, but rather a way to organise chronic patient treatment in a new organisational setup driven by PROM data, which supplement and support existing healthcare systems.
The ECM model sees through the establishment of a close collaboration between the chronic patient and the healthcare professionals, where the patient contributes with daily condition measurements, which, using telehealth technology, is immediately reported to a call centre.
The call centre staff and healthcare professionals use this information to react proactively and quickly in the event of changes or worsening of the condition over time. With the help of telehealth tools and dispensed medicine available at the patient home, the staff can subsequently carry out even difficult treatments right there. The close and real-time monitoring of the chronic patient’s condition and subsequent immediate interventions, when needed, results in constant adjustments of the chronic patient’s health status. For the COPD patient, this means that even small and early indications of inflammation, which can lead to a severe exacerbation, are addressed with an intervention that reduces or prevents the exacerbation.
When chronic patients are referred to treatment in their own homes based on the ECM model, the first step is to educate the patients and increase their health literacy. The next step is to introduce the ECM telehealth home kit, which consists of a tablet and medical devices. In the case of COPD patients, medical devices include a spirometer, a pulse-oximeter and a prescription of specific drugs used for severe acute exacerbations. As mentioned, enrolled patients measure and report their status 1-2 times every day, and this reporting enables the call centre staff to follow the patient’s condition and intervene when needed. After completing their daily reporting, patients also get an overview of their health status, and this increases the patient’s awareness, motivation, and compliance. Patients who are in ECM treatment are therefore generally more compliant and observant on taking their medicine correctly and on their lifestyle and exercises. The ECM model includes holistic measurements of mental well-being as part of the PROM data (based on the WHO-5 Well-Being Index), and this helps reduce patient anxiety and increase their mental health status.
Can a New Approach Reduce Costs and Benefit Chronic Patients?
Until recently, it was not clear whether telehealth treatment of patients in their own homes would lead to cost savings and benefits for the patients. Research and studies in Denmark based on large-scale telehealth projects document cost savings in the range of 1,000 € per chronic patient per year and that patients at the same time increase their quality of life – and achieve more healthy life years.
The ECM treatment model, which, as mentioned earlier, can be considered a newly designed mini healthcare system. It is, however, more powerful than traditional telehealth because the model is based on an optimised patient-centred approach and procedures. Preliminary results from ongoing research projects in Denmark to document the effects of the ECM organisational model indicate that the average cost associated with the treatment of a chronic COPD patient can be reduced by almost 50%. This is equivalent to an estimated saving per patient of 3,200 € per year vs. an average cost per COPD patient in the Danish healthcare system of 6,700 € per year.
The major contribution to this cost reduction is from avoidable visits and contacts with GPs, emergency departments, outpatient clinics and hospital admittance. If we take the study of a particular patient enrolled in the project as an example, the estimated savings related to avoidable hospital inpatient admittance amounts to 18,000 € for the first year of enrollment in the project. During the year leading up to enrollment in the project, the patient had 2.900 km transport related to GP, clinic and hospital visits, and this indicates that the agenda of telehealth and in-home remote treatment can also contribute to the climate agenda – and to saving chronic patients time related to transport.
The lung capacity chart below (a real-life example from an ECM patient) explains why it is possible to reduce clinic and hospital visits and at the same time improve the patient’s quality of life. From the chart, we can see the daily reporting from a patient, and we see that there are red columns in the beginning, after the patient has been enrolled. The red columns indicate low lung capacity or indication of exacerbation risk based on other monitoring parameters from the patient.
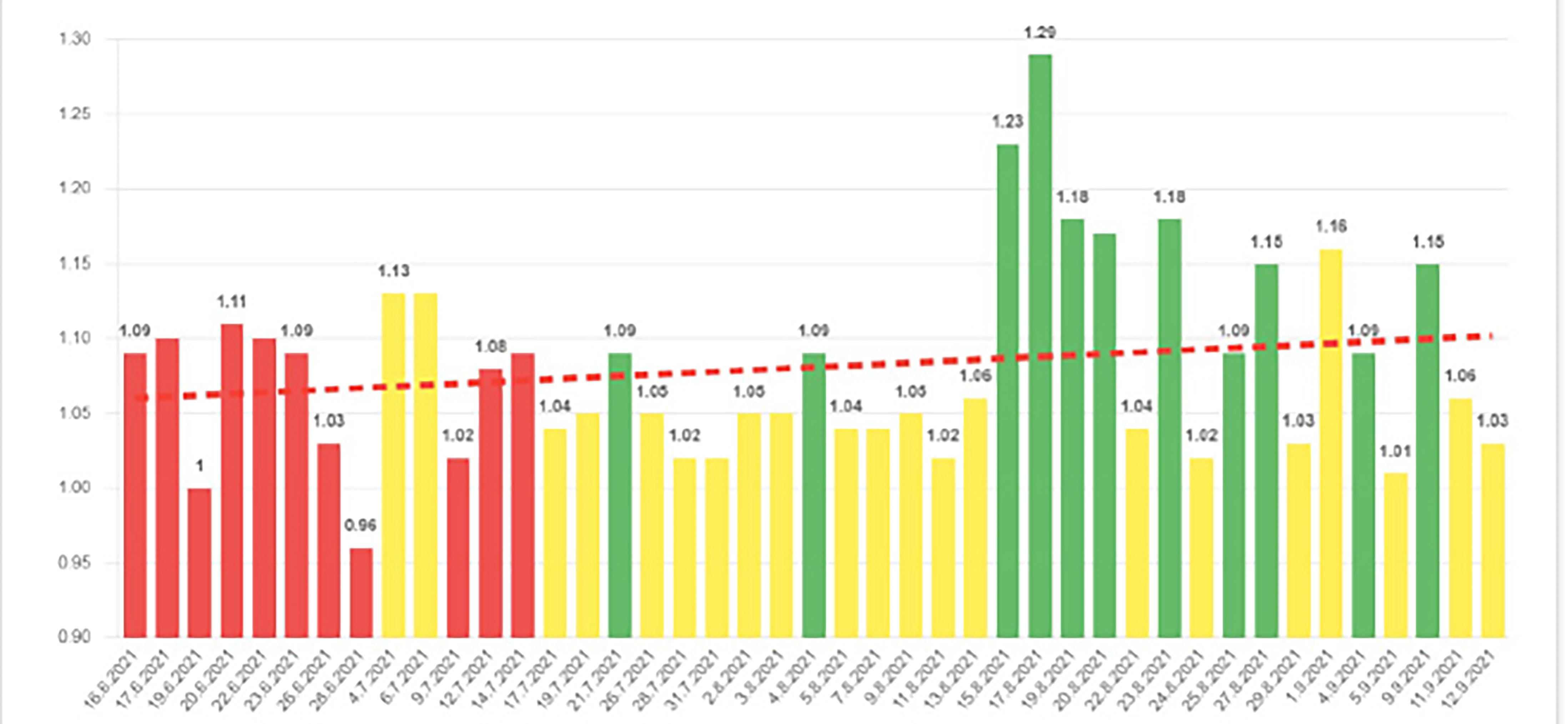
Gradually, as the clinical staff intervene, the medical in-home treatment of the patient leads to improvements, and the red columns over the following weeks changes to yellow and green, which indicate that the patient is now well regulated and not at risk of exacerbations. The dotted red line indicates the development of the lung capacity of the patient. It is not possible to cure COPD, but avoiding exacerbations can preserve lung capacity, increase the quality of life, and delay the development of the COPD disease.
Staff and Workforce Issues
A population that grows older and lives longer, resulting in more chronic diseases and comorbidity, means that demand for healthcare treatment increases. At the same time, a smaller proportion of the population will be of working age. In Europe, more than one-third of the population will be older than the age of 65 years by 2060, and this means that the working-to-age ratio will change from 1,86 to 1,25, meaning that there will only be 1,25 persons working in 2060 for each retired, elderly citizen.
The staff and workforce issues related to recruiting healthcare professionals are already a challenge in many countries. Increasing demands for healthcare services, but also more competition from new healthcare providers (e.g. Amazon Care, Microsoft and Google), will only increase the challenge in the coming years.
New models of care which reduce and avoid clinic visits and hospital admittance obviously reduce the need for healthcare professional intervention, and this means that more patients can be treated by the same medical staff. But – what about the medical staff needed to deliver in-home treatment?
The 6 step ECM model incorporates clear thresholds and procedures which allow certain tasks to be transferred to non-clinical staff in a secure and regulatory compliant way.

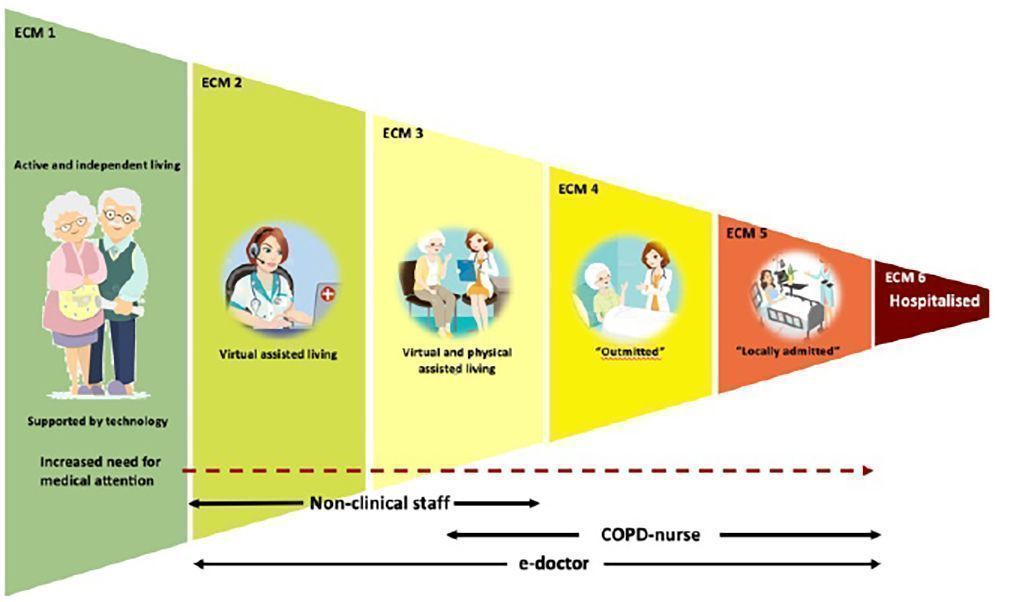
The 6 step Epital Care Model relies on increased health literacy and empowerment for chronic patients to manage their own compliance and health status in step 1. In step 2, call centre staff will reach out to patients based on their daily reporting. Call centre staff are non-clinical personnel who are authorised and certified to interact with patients based on ECM procedures. Procedures may require call-centre staff to involve physicians and nurses on duty (step 3), which can then be immediately involved in the patient dialogue. The ECM model also involves physical treatment of the patient in their home (nurse/physician visits – step 4) and forward sub-acute functions where a patient can be admitted (step 5). The overall responsibility for treatment always remains with the senior doctor, who can be contacted 24/7.
The experience from Denmark, where ECM treatment is in operation in certain local regions and for certain patients, is also that new models of care offer new career opportunities for nurses and physicians, and this can, of course be an important factor in the competition to attract the workforce needed in the future. The use of non-medical staff for simple monitoring tasks and standardised treatments controlled by well-documented algorithms - and with the overall treatment responsibility placed with the chief physician, is also an opportunity to add new resources to the health care system.
Wearables and Future Technology
Rumours suggest that the next generation of the Apple Watch will include functionality to measure blood sugar and that the next generation of the Samsung Watch will be able to measure the level of blood oxygen. So, do we need to establish telehealth projects based on current technology? Are we approaching a near future where we can just harvest the data from chronic patient wearables and, this way, achieve the same value and benefits?
New and emerging wearable technology is an opportunity to increase the cost savings from new models of care. The price of the ECM patient home kit is currently 450€, and if, e.g., pulse and blood oxygen levels in the near future can be measured with regulatory-approved wearable technology, this will reduce the price of the home kit to approximately 200€.
Technology alone does not lead to new models of care. There needs to be a re-design of the organisational setup which enables healthcare organisations to optimise the value which new technology can provide. And healthcare authorities need to offer technology platforms that can harvest data from wearables in a secure and regulatory-approved way to make such data available for the treatment of their patients.
The ECM model and technology platform can help healthcare authorities to initiate home treatment of chronic patients now, with a strategic opportunity to increase value and cost savings as new wearable technology is introduced in the coming years. 
Conflict of Interest
None.
References:
Epital Health – a disruptive and research-based approach to service transformation of health care systems. Available from https://ifsv.ku.dk/ansatte/?pure=da%2Fpublications%2Fepital-health--a-disruptive-and-research-based-approach-to-service-transformation-of-health-care-systems(d1856484-201f-486b-9951-f8c72b7f11c6)%2Fexport.html
Healthcare Innovation —The Epital: A Living Lab in the Intersection Between the Informal and Formal Structures. Available from https://publichealth.ku.dk/staff/?pure=en%2Fpublications%2Fhealthcare-innovation-the-epital(94c6b901-48dd-4218-9ada-91d631feb75d)%2Fexport.html
The Epital Care Model: A New Person-Centered Model of Technology-Enabled Integrated Care for People With Long Term Conditions. Available from https://publichealth.ku.dk/staff/?pure=en%2Fpublications%2Fthe-epital-care-model(99bdc166-e614-46ce-96d5-35f12f0fecb5)%2Fexport.html



