HealthManagement, Volume 16 - Issue 1, 2016
Healthcare, a Changing Landscape
Equal access to a quality healthcare system is part of the Canadian Charter of Rights and Freedoms (1982), and is considered as a right by Canadians. Making Canadians the healthiest people in the world as well as preserving a healthcare system that is true to their values and sustainable must be the system’s overriding objective (Royal Commission on the Future of Healthcare in Canada 2002). In 2007 the Lewis and Romanow report identified four priorities that the healthcare system had to address urgently:
- Waitlist management;
- Fiscal sustainability;
- Primary care reform;
- End-of-life care (Dickson 2008)
However, in 2014 the Commonwealth Fund reported that Canada’s healthcare system ranked 10th out of 11 developed countries, mainly due to safety, timeliness and efficiency of care (Davis et al. 2014).
A Report on Canadian’s Expectations of the HealthCare System, released at the National Health Leadership conference in June 2015, revealed that 70 percent of Canadians are very worried about being excluded from the system, especially when it comes to critical areas such as mental health, care of seniors, palliative care and hospital safety (HealthCareCAN 2015).
With an ageing population and finite financial resources, it is more than ever urgent to implement the steps required to bring Canada back into the top five in the next five years. A Call to Action issued at the Leadership conference identified as a key priority the need for better leadership by healthcare providers, as this is the first enabler of better health system performance and better organisational performance. It starts with individual leadership based on the needs of patients. It also means senior healthcare leaders working better together to plan and organise healthcare systems for the future.
In 2004 the Province of British Columbia identified the leadership gap in healthcare and called for new leadership skills in the healthcare system. The Health Care Leaders’ Association of British Columbia (HCLABC) joined forces with the Centre for Health Leadership and Research at Royal Roads University to define the concept of strategic leadership for healthcare reform. This resulted in the creation of Leaders for Life in 2006 and the introduction of the LEADS framework, the result of an action research study led by Professor Graham Dickson in October that year. LEADS in a Caring Environment rapidly gained national recognition and was endorsed by the Canadian Health Leadership network (CHLNET) (chlnet.ca) and the Canadian College of Health Leaders (cchl-ccls.ca) in 2009. That consortium of LEADS-based partners has grown to include most national health organisations, whole provinces, and multiple health agencies and or institutions in all provinces in Canada by 2016.
Leadership Crisis
Leadership has been identified as the single most important factor in the success of any enterprise. As stated by the Logan Arts Leadership Institute, “Real leadership is a precious commodity, and it is in increasingly short supply…” (interlochen.org/LoganArts).
The current leadership low supply crisis is primarily caused
by a massive retirement bulge of “baby boomers” and lack of succession
planning. Healthcare institutions are under pressure to improve performance,
safety and quality, which means major transformation in their operational
models. More and better leadership as performing now is not enough anymore. In
2007 the Conference of Deputy Ministers of Health in the Pan-Canadian Health
Human Resource Framework acknowledged as a national priority the need for
stronger leadership to attract and retain highly qualified people to work in
healthcare (Federal/Provincial/Territorial Advisory Committee on Health
Delivery and Human Resources 2007).
A leader is expected to innovate, inspire trust, challenge the status quo
Boosting Leadership Capacity
There are two ways to achieve stronger leadership capacity:
• Increase the Quantity (widespread): moving away from the old model of top-down leadership, this is the concept of distributed leadership, where more people at all levels will provide leadership, with widespread leadership accountability. However, this assumes the implementation of an extensive infrastructure for leadership development to build capacity.
• Improve the Quality (upgraded): this model requires enhancing the skills of leaders and helping them to acquire a set of competencies to become powerful through influence rather than authority and strategic in understanding and implementing the organisational vision and priorities, in order to achieve the transformation required by the system.
Both strategies must be developed in conjunction, as they complement each other.
Leadership versus Management
It is common to see confusion between leadership and management. Both are often addressed under the same banner, mainly in business school programmes. But they must be clearly differentiated:
• Leadership is the visionary quality required to drive change in a complex environment, that will set the direction and strategy expected by the group. A leader is expected to innovate, inspire trust and challenge the status quo.
• Management relies on a set of knowledge and skills required to organise, plan, evaluate and control when the direction has been defined. a manager is expected to administer, rely on control and accept the status quo.
The LEADS Framework
The LEADS framework (leadersforlife.ca/site/framework) represents the key skills, abilities and knowledge required to lead at all levels of an organisation. it aligns and consolidates the leadership strategies and competency frameworks found in Canada’s healthcare sector. The guiding principle behind LEADS is that leadership soft and hard skills can be defined and developed in order to increase the number and quality of leaders. The LEADS framework is simple, complete, portable, and can be applied to all levels.
There are five domains in the LEADS framework (Fig. 1):
- Lead Self;
- Engage Others;
- Achieve Results;
- Develop Coalitions;
- Systems Transformation.
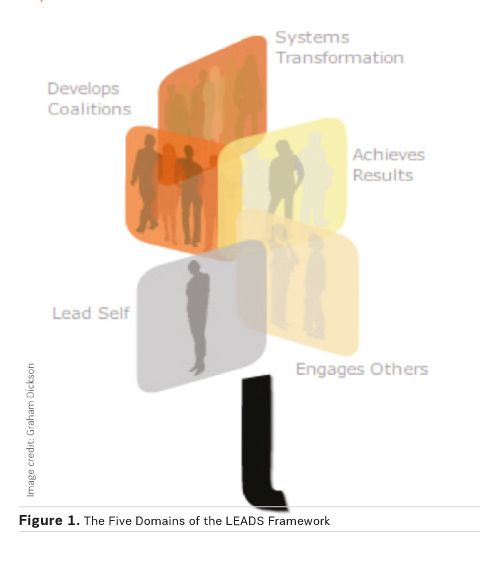
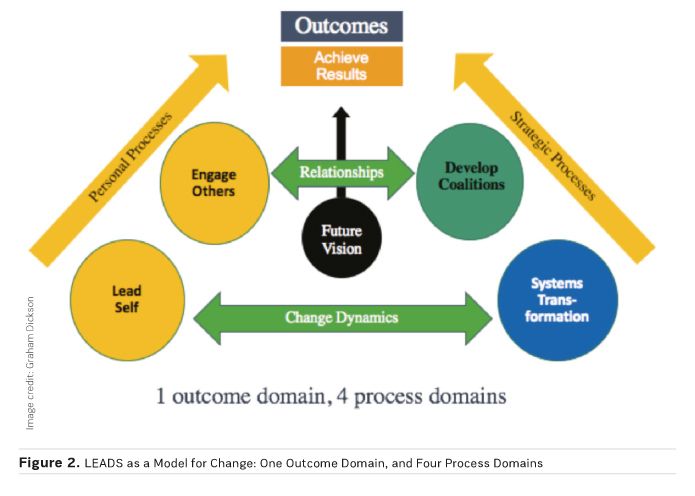
The domains interact with one another to create effective leadership and accomplish change (Fig. 2). Each domain is composed of four capabilities. Capabilities differ from competencies in the fact that they are organic, evolve and develop over time and are unique to each individual.
1. Lead Self
a. Self-aware: leaders must recognise their own emotions and the impact they may have on others. They must be aware of their perceptions and assumptions, as well as of the values and principles which will guide their decisions.
b. Manages self: leaders must demonstrate emotional self-control, initiative and optimism. Maintaining life balance is important, as leaders must be well equipped to deal with challenges.
c. Demonstrates character is composed of two major attributes: personal integrity and emotional resiliency, key to successful leadership.
d. Develops self: leaders must develop soft skills, such as confidence and social intelligence. Every experience must be an opportunity for lifelong learning.
2. Engage Others
a. Foster development of others: a good leader must recognise and reward the work and effort of others, coach, teach and encourage learning. The leader must deal with inappropriate behaviour.
b. Contribute to the creation of healthy organisations, in building trust, promoting safety, service and quality and ensuring resources are available for people to perform effectively.
c. Communicate effectively, starting with being a good listener, and use different communications media to convey a clear message. It is not uncommon for leaders to display poor communication skills and to assume that people will guess what they have in mind.
d. Build teams, in encouraging participation from stakeholders and finding ways to use people’s strengths. But priority must be given to articulate clearly the vision and goals.
3. Achieve Results
a. Set direction: a key role for a leader is to build a compelling vision for the future with clearly defined outcomes, and communicate this vision in an effective way, which is the only way to get commitment from those who need to be part of the plan moving forward.
b. Strategically align decisions with vision, values and evidence; this is not an easy task, taking into consideration the complexity of our healthcare system. We need to respect multiple factors such as culture, structure and personal skills.
c. Take action to implement decisions, with an absolute focus on results. The leader must command, but at the same time must be able to delegate and let go of the details.
d. Assess and evaluate: people must be accountable to standards of performance. Based on accurate data collection, the leader must use tools such as balanced scorecard or logic models to measure performance and achievements, and course correct if needed.
4. Develop Coalitions
a. Purposefully build partnerships and networks to create results: once the goals and objectives are clearly defined, choose the right partner and identify the right form of collaborative structure, built on trust and reciprocity, sharing risks and benefits.
b. Demonstrate a commitment to customers and service, and ensure that all partners remain true to the value proposition, in order to achieve desired outcomes. The caring purpose must be kept at the forefront, benefits to patients or citizens must be defined, and the coalition must measure progress to course correct along the way.
c. Mobilise knowledge, using the “five As” strategy: ask the right question, acquire the right information, assess the reliability of that information, adapt or repackage that information as necessary, and apply the evidence strategically.
d. Navigate sociopolitical environments: requires the leader to be politically astute, which means understanding threats and opportunities, being aware of key players and treating others with respect; the leader must build emotional resiliency to be able to negotiate through conflicts and mobilise support, handling uncertainty with confidence and influencing resistant partners to support a solution.
5. Systems Transformation
a. Demonstrate systems/critical thinking: of course, the leader must understand the pressing issues within our complex health system, challenge the status quo, and design and implement the process which will lead to systems transformation.
b. Encourage and support innovation, as this is the engine of creativity and can lead to success through evidence based approaches.
c. Orient themselves strategically to the future: the leader is expected to be the visionary, conscious of trends and issues, able to shape the future.
d. Champion and orchestrate change: this is the ultimate goal, where the leader has accomplished all the steps required to improve the health system performance and has aligned all the elements to execute change.
Conclusion
The Canadian healthcare system is in crisis, and requires major transformational changes to adapt to limited financial resources and an ageing population. Achieving this transformation means leadership at all levels, and leadership is a precious resource in short supply. We need to train more leaders, and LEADS in a Caring Environment (Dickson and Tholl 2014) has been designed to help healthcare professionals to acquire the soft and hard skills they need to implement all the steps required to achieve results and transform the current system. Leadership is an exciting journey and a lifelong learning experience, which must be practised at all levels of the organisation
Key Points
• Leadership is the single most important factor in the success of any enterprise.
• Better leadership is the first enabler of better health system performance.
• Leadership can be practised at all levels of the organisation.
• LEADS provides 5 domains and 20 capabilities to frame leadership.
• Leadership is a lifelong learning experience




