According to recent
findings published in the journal Proceedings
of the National Academy of Sciences, Professor Jonathan Stamler and
colleagues demonstrate that nitric oxide has the potential to reshape the way
we think about the respiratory system. Stamler, MD, is a Professor of Medicine
at Case Western Reserve University School of Medicine and Cardiologist at
University Hospitals Case Medical Center.
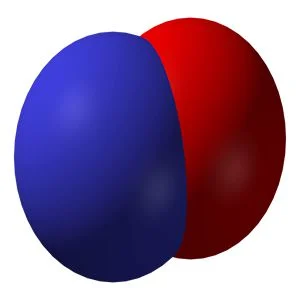
The traditional view is
that the respiration process involves two elements - oxygen and carbon dioxide
and the delivery of oxygen from lungs to tissues and the removal of carbon
dioxide is done through the process of exhalation. However, these new findings
report that nitric oxide is essential for the delivery of oxygen to the cells
and tissues. The findings also show that nitric oxide must accompany
haemoglobin to enable blood vessels to open and supply oxygen to tissues.
"The bottom line
is that we have discovered the molecular basis of blood flow control in the
respiratory cycle loop," Stamler said. "It's in the haemoglobin
protein itself, which has the ability to deliver the nitric oxide together with
oxygen. The simplified textbook view of two gases carried by haemoglobin is
missing an essential element - nitric oxide - because blood flow to tissues is
actually more important in most circumstances than how much oxygen is carried
by haemoglobin. So the respiratory cycle is actually a three-gas system."
In a previous research,
Stamler and his colleagues had revealed that the respiratory cycle was more
than an exchange of oxygen and carbon dioxide. They had also showed that red
blood cells carry and release nitric oxide. However, the exact physiologic
ramifications of nitric oxide release were not explained.
In this new research,
the investigators have uncovered the key role that nitric oxide plays in
controlling the blood flow in small vessels within tissues are responsible for
blood flow autoregulation. They examined the respiratory cycle in mice lacking
the one amino acid site that carries nitric oxide in their blood cells and
found that blood flow autoregulation was completely eliminated and the animals
could not oxygenate tissues.
The researchers found
that oxygen levels were low in the animals' muscles at baseline despite the
fact that their red blood cells were carrying a full load of oxygen. When the
mice were stressed for oxygen, the blood flow to their organs dropped
significantly. It was expected that this would prompt a spike in blood flow but
instead the reduced blood flow and oxygen shortfall triggered heart attacks and
heart failure in the nitric oxide-deficient animals.
The research thus demonstrates that nitric oxide-release mechanism regulates oxygen delivery. The historical belief that the control of blood flow is primarily through blood vessels and their endothelial linings is not entirely accurate because red blood cells also play a role. The tiny vessels and the red blood cells together control the process of blood flow. Stamler points out that red blood cell dysfunction could lead to diseases of the heart, lung and blood such as heart attack, heart failure, and stroke and ischaemic injury to kidneys.
Low levels of nitric
oxide in blood cells can cause blood disorders such as sickle cell anaemia.
Stamler concludes that blood flow cannot autoregulate without nitric oxide and
future therapies should focus on restoring red blood cell function, complete
with nitric oxide delivery capability.
Source: Case Western Reserve University
Image Credit: Wikimedia Commons