Results of a new modelling study published in Radiology showed that imaging could be a cost-effective tool for identifying people at risk for stroke who might benefit from aggressive intervention.
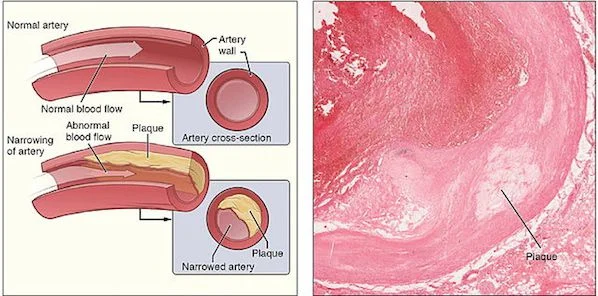
The study evaluated people with asymptomatic carotid artery stenosis, a narrowing of the major blood vessels transporting blood to the head due to atherosclerosis (i.e., plaque buildup). Data show that stenosis is the leading cause of up to 20 percent of ischemic strokes, which result from an obstruction within a blood vessel. Ischemic strokes account for 85 percent of all strokes.
It is common for stroke victims to undergo revascularisation procedures such as carotid endarterectomy, or surgical removal of the plaque, to restore blood flow. However, the use of such procedures in asymptomatic patients is "more controversial," said Ankur Pandya, PhD, assistant professor of healthcare policy and research and public health in radiology at Weill Cornell Medical College in New York City (USA).
“There are complications and costs associated with these revascularisation procedures," Dr. Pandya noted, adding that the procedures are often done without weighing whether the costs and risks are worth the benefits.
Prof. Pandya and colleagues assessed the impact of cerebrovascular reserve (CVR) testing, a measure of blood flow reserve to the brain, on asymptomatic people with significant carotid artery stenosis. They opted to use transcranial Doppler (TCD) sonography for the CVR testing, as TCD is an inexpensive imaging technique that does not expose patients to ionising radiation. The research team devised a mathematical model that allowed them to make hypothetical comparisons among three different approaches: CVR testing, immediate revascularisation with carotid endarterectomy, and medical therapy-based management with subsequent revascularisation only for patients whose stenosis got worse.
Key findings of the study include:
The results indicate that imaging can be a cost-effective tool to classify patients by risk of stroke and help assign patients to invasive, expensive interventions and less invasive options, said Prof. Pandya. In addition, CVR testing has the potential to help characterise whether carotid artery plaque is causing abnormal brain blood flow patterns which may then identify the patients who are at greatest risk of stroke.
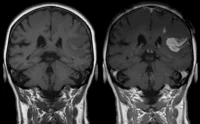
“CVR testing with ultrasound could be used to stratify patients by risk based on abnormal blood flow patterns to the brain, and then other imaging tests like MRI could be employed to look at the composition and stability of plaque, which may give greater insight into those plaques most likely to rupture and cause symptoms,” the professor explained.
Cost-effectiveness models such as the one used in the study have gained popularity in recent years and are already used by healthcare payers in Europe, Australia and Canada. These models should become more prominent in the US as healthcare reform evolves, Dr. Pandya said.
Source: Radiological Society of North America
Image Credit: Wikimedia Commons
The study evaluated people with asymptomatic carotid artery stenosis, a narrowing of the major blood vessels transporting blood to the head due to atherosclerosis (i.e., plaque buildup). Data show that stenosis is the leading cause of up to 20 percent of ischemic strokes, which result from an obstruction within a blood vessel. Ischemic strokes account for 85 percent of all strokes.
It is common for stroke victims to undergo revascularisation procedures such as carotid endarterectomy, or surgical removal of the plaque, to restore blood flow. However, the use of such procedures in asymptomatic patients is "more controversial," said Ankur Pandya, PhD, assistant professor of healthcare policy and research and public health in radiology at Weill Cornell Medical College in New York City (USA).
“There are complications and costs associated with these revascularisation procedures," Dr. Pandya noted, adding that the procedures are often done without weighing whether the costs and risks are worth the benefits.
Prof. Pandya and colleagues assessed the impact of cerebrovascular reserve (CVR) testing, a measure of blood flow reserve to the brain, on asymptomatic people with significant carotid artery stenosis. They opted to use transcranial Doppler (TCD) sonography for the CVR testing, as TCD is an inexpensive imaging technique that does not expose patients to ionising radiation. The research team devised a mathematical model that allowed them to make hypothetical comparisons among three different approaches: CVR testing, immediate revascularisation with carotid endarterectomy, and medical therapy-based management with subsequent revascularisation only for patients whose stenosis got worse.
Key findings of the study include:
- The CVR-based strategy, which led to about half of the patients receiving revascularisation, seemed to have the most favourable balance of benefits and costs.
- A medical therapy-based approach was associated with the lowest lifetime costs and the fewest revascularisations. However, it also resulted in the lowest life expectancy and lifetime quality-adjusted years, which account for both the length and quality of life experienced by patients.
- Immediate revascularisation had the highest costs by a wide margin, and only incremental health benefits compared with the CVR-based approach.
The results indicate that imaging can be a cost-effective tool to classify patients by risk of stroke and help assign patients to invasive, expensive interventions and less invasive options, said Prof. Pandya. In addition, CVR testing has the potential to help characterise whether carotid artery plaque is causing abnormal brain blood flow patterns which may then identify the patients who are at greatest risk of stroke.
“CVR testing with ultrasound could be used to stratify patients by risk based on abnormal blood flow patterns to the brain, and then other imaging tests like MRI could be employed to look at the composition and stability of plaque, which may give greater insight into those plaques most likely to rupture and cause symptoms,” the professor explained.
Cost-effectiveness models such as the one used in the study have gained popularity in recent years and are already used by healthcare payers in Europe, Australia and Canada. These models should become more prominent in the US as healthcare reform evolves, Dr. Pandya said.
Source: Radiological Society of North America
Image Credit: Wikimedia Commons
Latest Articles
atherosclerosis, ischemic stroke, revascularisation, carotid endarterectomy
Results of a new modelling study published in Radiology showed that imaging could be a cost-effective tool for identifying people at risk for stroke who mi...