Aside from making surgery safer for children with congenital heart disease, 3D printing technology can reduce the duration as well as the number of invasive procedures required — thus minimising healthcare costs. A case in point is when a cardiac surgeon in the US recently used a 3D printed heart as a model to plan a life-saving procedure for his young patient.
The child, Esther Perez, was born with a rare, life-threatening cardiac defect. Her doctor, Richard Kim, a cardiac surgeon at Children's Hospital Los Angeles (CHLA), pointed out, "Instead of opening the chest and making a decision about how to proceed, I could immediately begin fixing the problem." Usually, surgeons are not able to determine their approach until they open the chest, put the child on a heart bypass machine, survey the problem and then, make a quick decision on how to proceed with repair.
The variation in normal anatomy is increased in hearts with congenital abnormalities, hence an exact replica (a 3D roadmap) is very useful for surgeons to strategise before entering the operating room. "A 3D model allowed me to plan the surgery in advance, which meant Esther spent less time in surgery and received less anaesthesia — making the procedure safer," said Dr. Kim, who is also an assistant professor at the Keck School of Medicine of the University of Southern California.
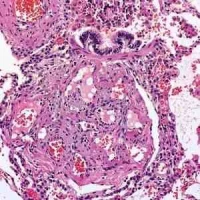
Jon Detterich, MD, a paediatric cardiologist who specialises in noninvasive cardiac imaging, explained that 3D printing technology can create an object of any shape by printing layer upon layer, using plastics or other materials in place of ink. He gathered both 2D and 3D MRI scans then translated the information into a format that could be read by a 3D printer. "As useful as scans are for visualising structural defects, there's nothing like holding a life-sized, three-dimensional replica in your hands," said Dr. Detterich, who is also an assistant professor at the Keck School of Medicine of USC.
To date, only a small number of 3D models have been used for heart surgery, "so it's too soon to tell if they improve surgical outcomes," said Frank Ing, MD, chief of Cardiology and co-director of the Heart Institute at CHLA. "But our experience suggests that using models saves time in the OR — which means increased safety and decreased costs." Dr. Ing is also a professor at the Keck School of Medicine of USC.
This knowledge about the benefits of using 3D models will likely translate into a need for fewer surgeries, and allow children — like Esther Perez — to spend less time recuperating in intensive care. Esther, who would have required multiple surgeries during the first years of her life, made a rapid recovery and is expected to look forward to a life free of medical complications.
CHLA has been named the best children’s hospital on the U.S. West Coast and amongst the top five in the country for clinical excellence with its selection to the prestigious U.S. News & World Report Honor Roll. It is also one of America's premier teaching hospitals through its affiliation since 1932 with the Keck School of Medicine of USC.
Source: Children's Hospital Los Angeles
Image Credit: Children's Hospital Los Angeles
The child, Esther Perez, was born with a rare, life-threatening cardiac defect. Her doctor, Richard Kim, a cardiac surgeon at Children's Hospital Los Angeles (CHLA), pointed out, "Instead of opening the chest and making a decision about how to proceed, I could immediately begin fixing the problem." Usually, surgeons are not able to determine their approach until they open the chest, put the child on a heart bypass machine, survey the problem and then, make a quick decision on how to proceed with repair.
The variation in normal anatomy is increased in hearts with congenital abnormalities, hence an exact replica (a 3D roadmap) is very useful for surgeons to strategise before entering the operating room. "A 3D model allowed me to plan the surgery in advance, which meant Esther spent less time in surgery and received less anaesthesia — making the procedure safer," said Dr. Kim, who is also an assistant professor at the Keck School of Medicine of the University of Southern California.
Jon Detterich, MD, a paediatric cardiologist who specialises in noninvasive cardiac imaging, explained that 3D printing technology can create an object of any shape by printing layer upon layer, using plastics or other materials in place of ink. He gathered both 2D and 3D MRI scans then translated the information into a format that could be read by a 3D printer. "As useful as scans are for visualising structural defects, there's nothing like holding a life-sized, three-dimensional replica in your hands," said Dr. Detterich, who is also an assistant professor at the Keck School of Medicine of USC.
To date, only a small number of 3D models have been used for heart surgery, "so it's too soon to tell if they improve surgical outcomes," said Frank Ing, MD, chief of Cardiology and co-director of the Heart Institute at CHLA. "But our experience suggests that using models saves time in the OR — which means increased safety and decreased costs." Dr. Ing is also a professor at the Keck School of Medicine of USC.
This knowledge about the benefits of using 3D models will likely translate into a need for fewer surgeries, and allow children — like Esther Perez — to spend less time recuperating in intensive care. Esther, who would have required multiple surgeries during the first years of her life, made a rapid recovery and is expected to look forward to a life free of medical complications.
CHLA has been named the best children’s hospital on the U.S. West Coast and amongst the top five in the country for clinical excellence with its selection to the prestigious U.S. News & World Report Honor Roll. It is also one of America's premier teaching hospitals through its affiliation since 1932 with the Keck School of Medicine of USC.
Source: Children's Hospital Los Angeles
Image Credit: Children's Hospital Los Angeles
Latest Articles
anaesthesia, heart surgery, MRI scans, congenital heart defects, 3D printing
Aside from making surgery safer for children with congenital heart disease, 3D printing technology can reduce the duration as well as the number of invasiv...