HealthManagement, Volume 2 - Issue 1, Spring 2008
Despite the implementation of several clinical guidelines, current strategies for the assessment of syncope vary widely among physicians and hospitals. Evaluation and treatment of syncope is often haphazard and unstratified. This results in the inappropriate use of diagnostic tests and in a number of misdiagnosed and still unexplained syncope.
The utilisation of medical resources and the expenses associated
with syncope management are enormous. Assuming the status quo of syncope evaluation
is left in its present state, the effectiveness of diagnosis and treatment is
unlikely to substantially improve. Even implementation of the published syncope
management guidelines is likely to be diverse, uneven in application, and of
uncertain benefit. Guidelines from scientific societies should provide the
standard, but are poorly known and sometimes difficult to apply in clinical
practice. Also, physicians from specialties different to those that created the
guidelines are reluctant to apply it to their patients. Thus, guidelines alone
will hardly change standard practice.
A prospective, observational registry from a sample of 28
general hospitals was performed in Italy in order to evaluate the impact of the
guidelines of the European Society of Cardiology (ESC) on the management of
syncope admitted in emergency. The Evaluation of Guidelines in Syncope Study 1
(EGSYS-1) enrolled all consecutive patients referred to their emergency rooms
from November 5, 2001 to December 7, 2001 who were affected by transient loss
of consciousness as the principal symptom. The findings of each of the 28
hospitals participating in the survey were evaluated separately.
Study Fails to Identify Uniform Syncope Practices
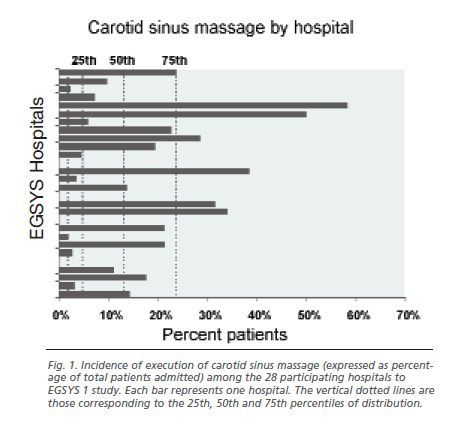
The authors observed great inter-hospital and inter-department heterogeneity regarding the incidence of emergency admission, in-hospital pathways, most of the examinations performed and the final diagnosis. For example, the execution of carotid sinus massage ranged from 0% in one hospital to 58% in another (median 12.5%) (see fig. 1); tilt testing ranged from 0% to 50% (median 5.8%) and the final diagnosis of neutrally mediated syncope The utilisation of medical resources and cope ranged from 10% to 78.6% (median 43.3%). As a consequence of the great inter-hospital variability, the authors were unable to describe a uniform strategy for the management of syncope.
This heterogeneity was minimally explained by a difference in
the clinical characteristics of the population referred to by the hospitals participating
in the study. Indeed, the proportion of explained variability was calculated to
be less than 10% of total variance. Thus, we can assume that the main
determinant of this different behaviour lies in the different attitudes of the
staff.
Therefore, what can one do? The solution is the creation of
standardised care pathways in which guidelines can be effectively applied.
New Strategy
The Evaluation of Guidelines in Syncope Study 2 (EGSYS-2) validated a new method of management for syncope based on a decision-making approach developed in strict adherence to the recommendations of the updated guidelines of the ESC in 465 patients from 11 general hospitals. In order to maximise its application, a decision-making guide line based software was used and trained core medical personnel were designated – both locally in each hospital and centrally – to verify adherence to the diagnostic pathway and give advice on its correction.
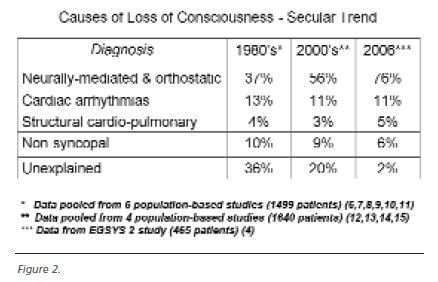
The results of this study probably assessed the current standard for the management of syncope and provided a frame of reference for daily activity when dealing with syncope. As a consequence of these methodological features, the results markedly differed from those of previous investigations; more diagnosis of neurally-mediated syncope were made and much less syncope remained unexplained than in the past (see fig. 2).
A prospective, controlled, multi-centre study was performed in
order to verify if this standardised method of care is feasible in the real
world and superior to the usual care. The patients referred from October 4 to
November 5, 2004 for emergency care, to 19 Italian general hospitals were
managed according to this new standardised care pathway and were compared with
those of EGSYS-1 referred from November 5 to December 7, 2001 who were managed according to the usual practices. There
were 929 patients in the usual care group and 745 patients in the standardised
care group. The baseline characteristics of the two study populations were
similar.
Study Underpins Guidelines
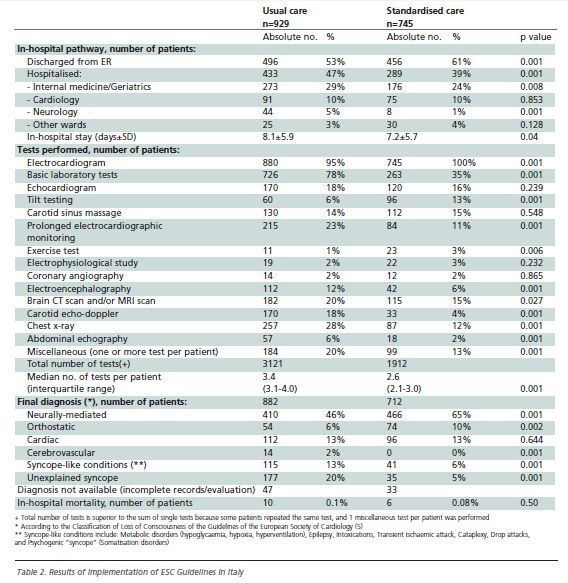
At the end of the evaluation, 78% of the patients assigned to
the standardised care group adhered to the guideline-based evaluation
achieving, when compared to usual care, 17% less hospitalisation rate (39% vs
47%), 11% shorter in-hospital stay (7.2±5.7 vs 8.1±5.9 days) and 26% fewer
tests performed per patient (median 2.5 vs 3.4). Forty-one percent more standardised
care patients had a diagnosis of neurally-mediated (65% vs 46%) and 66% more of
orthostatic (10% vs 6%) while 54% fewer had a diagnosis of pseudo-syncope (6%
vs 13%) and 75% fewer of unexplained syncope (5% vs 20%) (see table 2). The
mean cost per patient was 19% lower (1127 euros vs 1394 euros) and the mean
cost per diagnosis was 29% lower (1240 euros vs 1753 euros) in the standardised
care group (see table 1).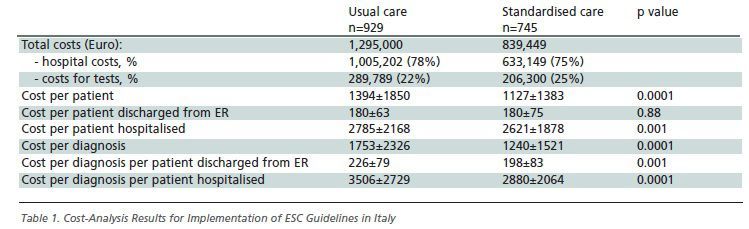
Thus, this study showed that a standardised care pathway significantly improved diagnostic yield and reduced hospital admissions, resource consumption and overall costs. Although the results of this study are difficult to reproduce in everyday practice, the study shows that ESC guidelines can be implemented in the clinical setting, provided the presence of trained medical personnel and the use of specifically designed decision-making software are in place. Thus, these results support the creation of cohesive, structured syncope facilities, as in the model proposed by the ESC guidelines in order to provide optimal quality service on the basis of well-defined, up-to-date diagnostic guidelines.






