Adding digital twin-guided ablation to standard pulmonary vein isolation (PVI) significantly improved outcomes in patients with persistent atrial fibrillation (AF), according to late-breaking results from the CUVIA-PRR trial presented at ESC Congress 2025.
AF affects one in three adults worldwide and is characterised by fast, irregular heartbeats. For patients in whom anti-arrhythmic drugs (AADs) fail, catheter ablation is a standard treatment that destroys small areas of cardiac tissue triggering the arrhythmia.
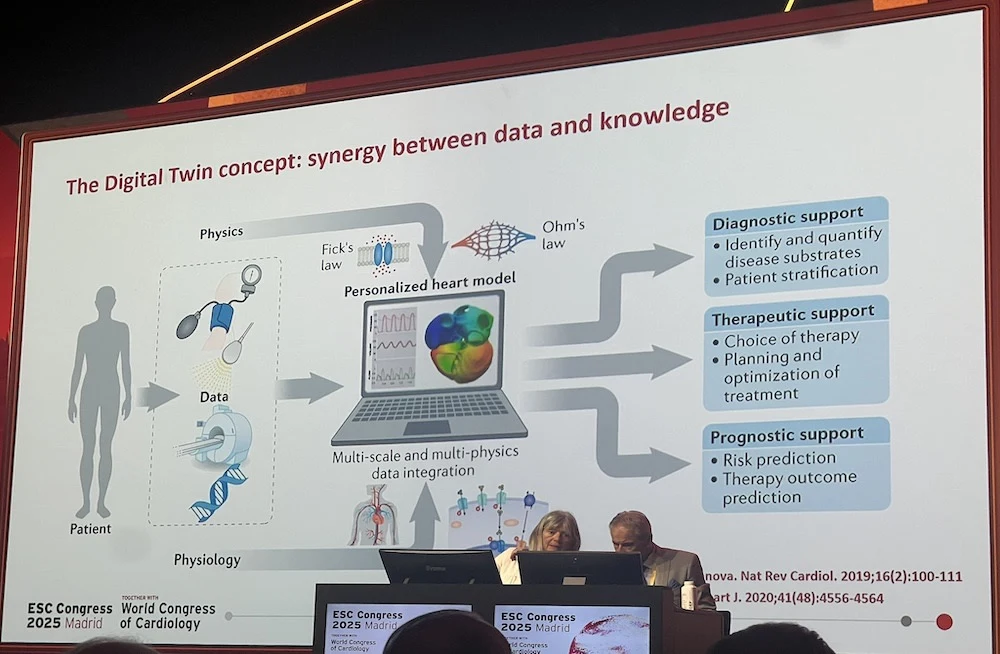
PVI is the cornerstone of AF ablation, but its effectiveness is limited in patients with persistent AF. Study researchers developed a personalised method using digital twin technology to identify patient-specific atrial areas, called phase singularity (PS) points, that sustain AF in simulations. They then tested whether adding ablation of these PS points to PVI would improve outcomes.
The trial was conducted at four centres in South Korea and enrolled patients with persistent AF refractory to AADs undergoing first-time ablation. Patients were randomised 1:1 to PVI alone or PVI plus digital twin-guided ablation of stable PS points. Maps identifying PS points were generated before PVI in the intervention arm. AADs were permitted during the 3-month post-ablation blanking period but discouraged thereafter. The primary endpoint was any documented atrial arrhythmia ≥30 seconds after the blanking period, with or without AADs.
A total of 304 patients were randomised and completed the blanking period (median age 61.3 years; 20.7% women). Stable PS points were identified and ablated in 43.2% of patients assigned to the digital twin-guided group.
At 18 months, arrhythmia-free survival was significantly higher with digital twin-guided ablation plus PVI compared with PVI alone (77.9% vs 59.5%). Freedom from arrhythmia without AADs was also greater in the digital twin-guided group (45.7% vs 31.7%). AAD use beyond 3 months was lower in the digital twin-guided group (51.6% vs 63.8%). Complication rates and total procedure times were similar between groups (142 vs 137 minutes).
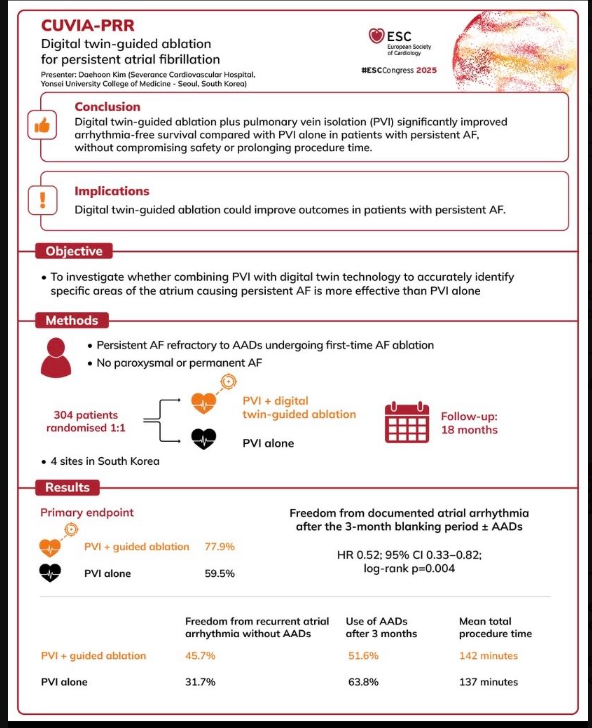
These findings show that in patients with persistent AF, digital twin-guided ablation added to PVI significantly improved arrhythmia-free survival without increasing risk or prolonging procedures. Unlike prior approaches that applied uniform ablation strategies or AI guidance that extended procedure time, this tailored, patient-specific method effectively targeted the mechanisms sustaining AF.
Source: ESC
Image Credit: ESC