Pulmonary imaging methods like chest radiography (CXR) and chest CT scans provide static views of the respiratory cycle, while pulmonary function tests (PFTs) offer essential physiological data but lack anatomical detail and can be challenging to perform, especially during disease exacerbations. Dynamic digital radiography (DDR) captures lung movement during respiration, providing a dynamic view of lung and diaphragm motion with radiation exposure comparable to traditional imaging methods. Although manual DDR-image analysis is labor-intensive, an automated analysis pipeline has been developed to calculate DDR-based projected lung areas (PLAs).
Previous studies have shown correlations between PLAs from DDR and traditional lung function metrics like total lung capacity (TLC) and vital capacity (VC). These correlations suggest DDR could serve as a surrogate for PFTs. The study aimed to evaluate the correlations between traditional PFT volumes and DDR-based PFT (dPFT) areas using a convolutional neural network (CNN) analysis pipeline to quantify lung areas in DDR sequences. Strong correlations were observed between traditional PFT and dPFT measures, with dPFT-based strain analysis effectively capturing lung physiology in conditions like COPD and restrictive diseases. A recent study published in CHEST Pulmonary investigates the potential of an automated machine learning DDR analysis pipeline to create dPFTs, providing a dynamic and less burdensome alternative to traditional PFTs.
Patient Recruitment and Protocol for Pulmonary Function Testing
Patients were recruited from two hospitals during outpatient pulmonary appointments, with exclusion criteria including those under 18 years of age, pregnant or lactating individuals, and those unable to consent independently. Additionally, patients who could not undergo both pulmonary function tests (PFTs) and dynamic digital radiography (DDR) within 150 days were excluded, as well as those experiencing disease exacerbations, changes in management, or new diagnoses during this period. Ultimately, 55 participants completed both PFT and DDR studies.
During DDR, patients followed a breathing protocol involving two tidal respirations, one maximal inspiration and expiration, and subsequent tidal breathing. This protocol closely approximates slow vital capacity (VC) acquisition. PFTs were conducted according to American Thoracic Society standards, measuring total lung capacity (TLC), VC, FEV1 % predicted, tidal volume, inspiratory capacity (IC), and functional residual capacity (FRC). DDR sequences were captured using Konica Minolta machines at 15 frames per second, with radiation exposure levels comparable to standard chest X-rays.
Automated Image Processing and Analysis Pipeline for Dynamic Digital Radiography
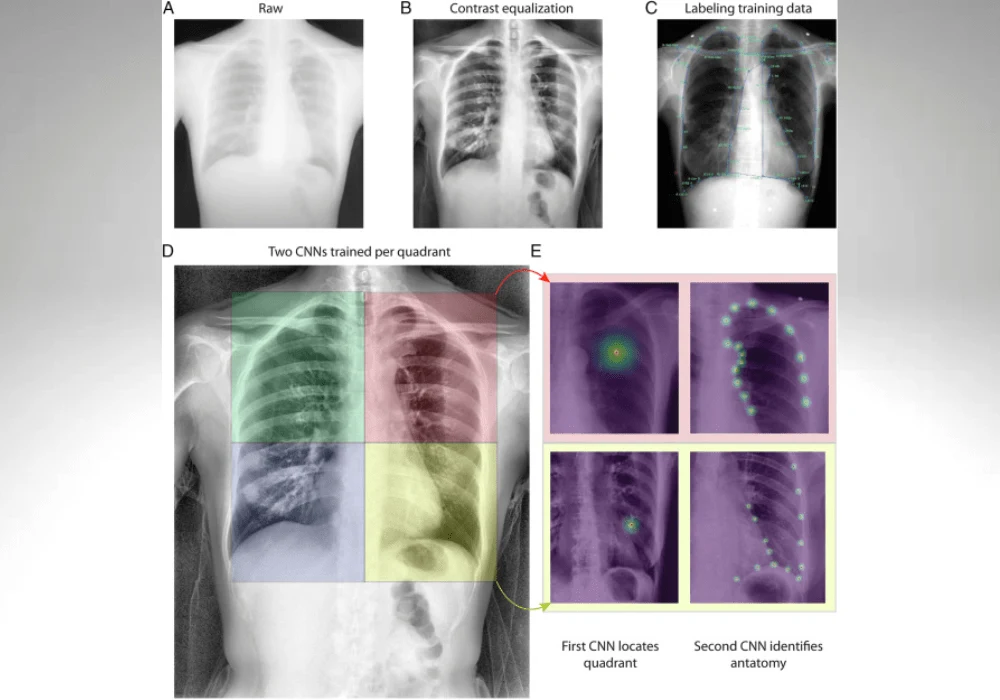
For image processing, a contrast adaptive local histogram equalization filter (CLAHE) was applied, and images were labeled with 61 anatomical points. Convolutional neural networks (CNNs) were trained using Social LEAP Estimates Animal Pose (SLEAP) software, with a top-down approach applied to each of four lung quadrants to achieve optimal performance. Poor tracking frames, often due to high BMI, were manually curated and excluded from analysis.
Lung areas were calculated using custom Python software by summing pixels within polygons for each anatomical structure. Flow rates were quantified by analyzing framewise area changes after Gaussian smoothing. Strain plots were generated by measuring distances between anatomical point pairs, with positive percent change indicating inhalation and negative percent change indicating exhalation. Pearson regressions and polynomial regressions were used to analyze the data, with strain analysis highlighting lung physiology in various conditions.
Exclusion Criteria, Analysis Methods, and Data Visualization for Dynamic Digital Radiography Study Ninety-nine patients underwent dynamic digital radiography (DDR), but 14 were excluded due to incomplete pulmonary function tests (PFTs), 16 due to poor DDR quality, 11 for not meeting the 150-day criteria between DDR and PFTs, and three for suboptimal PFTs, leaving 55 cases for the final analysis. Lung volume measurements were obtained via whole-body plethysmography in 45 patients and gas dilution in 10. Power calculations indicated sample size requirements of 16 for vital capacity (VC) and 25 for forced expiratory volume (FEV1) based on previous PLA correlations.
In the analysis, Gaussian smoothing was applied to each point across adjacent frames, allowing the calculation of left lung, right lung, and heart areas, producing lung area-time plots. These plots are analogous to PFT volume-time plots and included area-flow plots to represent area change per second, similar to PFT flow-volume loops. Peak detection tracked inhalation peaks and exhalation troughs, generating triggered-flow plots and lung-area plots. Unlike traditional PFTs, DDR captures anatomical changes, enabling strain analysis, which shows framewise percent changes depicting relative chest expansion and contraction during respiration.
Comparative Physiological Analysis and Correlation of DDR-based PFTs with Traditional Measures
Physiological differences were illustrated with three cases: normal, COPD, and restrictive disease. Lung area-time plots demonstrated distinct dynamic ranges during peak inhalation and exhalation, with flow-area loops showing higher values in COPD, consistent with hyperinflation, and diminished volumes in restrictive cases. Strain and grouped strain plots indicated greater dynamic range for normal lungs compared to COPD and restrictive examples. Breath-triggered flow plots showed faster area changes for normal physiology, while flow-area density plots highlighted class differences, with leftward shifts and decreased lung areas in restrictive cases and rightward shifts indicating COPD hyperinflation.
To assess the reliability of DDR-based PFTs (dPFTs) as surrogates for traditional PFTs, correlations between PFT volume measures and analogous dPFT area measures were analyzed. Maximum lung areas strongly correlated with PFT TLC, and the difference between maximum and minimum lung areas correlated with PFT VC. DDR-based flow changes correlated with FEV1, while DDR-analogous inspiratory capacity (IC) and functional residual capacity (FRC) measures also showed strong correlations with their PFT counterparts. These correlations suggest that dPFTs might reliably substitute traditional PFTs.
Functional Analysis of Lung Dynamics and Diaphragm Movement Using DDR-Based PFTs
Strain analysis identified respiratory dynamic differences among patients with normal, COPD, and restrictive physiologies. Normal lung physiology showed the most strain at the start of the largest exhale, while restrictive physiology demonstrated reduced rib movement but increased diaphragm movement. COPD physiology exhibited less lung contraction during inhalation. The lung area-to-regional strain relationship indicated that normal lungs had the largest dynamic ranges for both lung area and strain, while restrictive physiology had decreased ranges, particularly in bilateral rib cage movement.
A curvature index, defined as the vertical-to-horizontal diaphragm radius ratio, was created to quantify diaphragm movement. This index showed that both COPD and restrictive patients had lower curvature indices, indicative of flatter diaphragms. Pulmonary reserve, representing the percent of lung area used during tidal breathing relative to maximum VC, was introduced to categorize lung conditions and quantify spare lung function. Both COPD and restrictive conditions exhibited lower pulmonary reserve values compared to normal physiology.
To further differentiate pulmonary conditions, pulmonary reserve values were compared with DDR-based VC-to-flow ratios. Normal lungs, having large area changes and high flows, exhibited high pulmonary reserve and VC-to-flow ratios. COPD lungs, with limited dynamic area range and temporary high flows, had smaller VC-to-flow ratios, while restrictive lungs, with decreased compliance and short, high-intensity flows, had the smallest VC-to-flow ratios. These differences suggest that dPFT measures can effectively distinguish between normal and abnormal lung physiologies.
Clinical Implications for Advancing Pulmonary Function Assessment
Dynamic Digital Radiography (DDR) provides valuable insights into dynamic lung functioning, but manual analysis is time-consuming. The automated analysis pipeline generates DDR-based pulmonary function tests (dPFTs), offering a potential alternative to traditional PFTs. The strong correlations between PFTs and dPFTs demonstrate a significant relationship, suggesting dPFTs can reliably estimate key PFT measures like TLC, VC, FEV1, IC, and FRC.
DDR uniquely captures the dynamic interactions between the lungs, diaphragm, and heart throughout the breathing cycle while minimizing radiation exposure. Findings suggest DDR can serve as a functional study tool, enabling visualization of respiratory dynamics and providing strain analysis, which is not possible with traditional PFTs. Diaphragm motion, crucial in pulmonary disorders, is particularly well-captured with our multipoint tracking and curvature index for diaphragm shape quantification.
dPFTs are advantageous for patients who cannot complete traditional PFTs due to conditions like neuromuscular disorders or during disease exacerbations. The ease of DDR acquisition supports its feasibility for longitudinal studies, potentially identifying treatment needs by tracking changes in dPFTs and pulmonary reserve over time. Portable DDR machines could also facilitate emergency evaluations, particularly during COPD exacerbations.
However, limitations include the study's small sample size and specific patient population, the variability in lung volume measurement methods, and the need for improved standardization during DDR acquisition. Future studies should include more diverse and complex cases, incorporate both PA and lateral DDR sequences, and explore enhanced diaphragm tracking methods.
Overall, the study highlights the potential of dPFTs for assessing lung dynamics and suggests DDR as a valuable tool when traditional PFTs are impractical. This automated analysis could significantly enhance pulmonary function evaluation in various clinical settings, particularly for monitoring dynamic physiological changes over time and during disease flares.
Source & Image Credit: CHEST Pulmonary