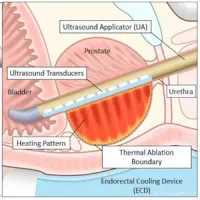
In a single-centre cohort study of 1,020 men who underwent both biparametric targeted and standard transrectal ultrasound-guided biopsies, low-suspicion biparametric magnetic resonance imaging (bpMRI) had a high negative predictive value (97%) in ruling out significant prostate cancer on confirmatory biopsies. The findings are published online in JAMA Network Open.
The study was conducted by Lars Boesen, MD, PhD, Department of Urology, Herlev Gentofte University Hospital (Denmark) and colleagues. Suspicion grades of bpMRI, biopsy results, and negative predictive value (NPV) of bpMRI were evaluated for detection of or ruling out significant prostate cancer (Gleason score 4 + 3 or maximum cancerous core length >50% for Gleason score 3 + 4).The researchers compared the diagnostic performance of standard biopsies in all men with standard plus targeted (combined) biopsies restricted to men with suspicious bpMRI findings. The reference standard was combined biopsy results from all men.
Study patients had a median age of 67 years (interquartile range, 61-71 years) and a median prostate-specific antigen (PSA) level of 8.0 ng/mL (interquartile range, 5.7-13.0 ng/mL). Combined biopsies detected any and significant prostate cancer in 655 of 1,020 men (64%) and 404 of 1,020 men (40%), respectively. Restricting combined biopsies to men with suspicious bpMRI findings meant 305 of 1020 men (30%) with low-suspicious bpMRIs could avoid prostate biopsies (biopsy in 715 men with suspicious bpMRIs vs. all 1020 men who required standard biopsies [70%]; P < .001).
Biparametric MRI offers the advantage of a relatively short imaging time versus the widely used multiparametric MRI and does not require intravenous contrast administration. Based on their findings, Dr. Boesen and colleagues recommended bpMRI as a risk stratification tool to exclude aggressive disease and unnecessary biopsies.
In a linked commentary, Timothy J. Wilt, MD, MPH, and Philipp Dahm, MD, MHSc, both with Minneapolis Veterans Affairs Health Care System, University of Minnesota School of Medicine, Minneapolis, MN, say that Boesen et al.'s approach (i.e., bpMRI method as a triage test) may mitigate physical, psychological, and financial harms of prostate cancer detection and treatment strategies that rely on widespread PSA testing, blind systemic biopsies for men suspected of having prostate cancer based on PSA results and/or abnormal digital rectal examination results, and treatment of most identified cancers.
While Boesen's study placed great emphasis on the sensitivity (98%) and negative predictive value (97%), the commentators say it is also important to consider the less impressive specificity (48%) and positive predictive values (56%). "Based on the authors’ findings, we calculated that for every 1,000 men who underwent bpMRI, 311 patients would be told they have a lesion concerning for prostate cancer, increasing their anxiety," Drs. wilt and Dahm point out.
While the commentary highlights the need for further external validation of the findings of Boesen and colleagues and others with multiparametric MRI, nonetheless, Drs. Wilt and Dahm say the rise of modern MRI is a potentially positive development, offering at-risk men the opportunity to decrease unnecessary and harmful biopsies.
"However, for MRI-based triaging strategies to be cost-effective, patients and physicians must be willing to change management based on MRI findings (i.e., decrease additional tests and treatments) rather than using MRI as an add-on to identify, upgrade, and treat more patients with prostate cancer," the commentators explain.
Source: JAMA Network Open
Image Credit: BQmUB2012102
References:
Boesen L et al. (2018) Assessment of the Diagnostic Accuracy of Biparametric Magnetic Resonance Imaging for Prostate Cancer in Biopsy-Naive Men: The Biparametric MRI for Detection of Prostate Cancer (BIDOC) Study. JAMA Network Open. 2018;(2):e180219. doi:10.1001/jamanetworkopen.2018.0219
Wilt TJ, Dahm P (2018) Magnetic Resonance Imaging–Based Prostate Cancer Screening: Is High-Value Care Achieved or Does the Holy Grail Remain Elusive?
JAMA Network Open. 2018;1(2):e180220. doi:10.1001/jamanetworkopen.2018.0220
Latest Articles
prostate cancer, prostate cancer detection, Biparametric MRI, bpMRI
In a single-centre cohort study of 1,020 men who underwent both biparametric targeted and standard transrectal ultrasound-guided biopsies, low-suspicion biparametric magnetic resonance imaging (bpMRI) had a high negative predictive value (97%) in ruling o