The journal Radiology has published online the findings of a new multicenter study entitled "Coronary Artery Plaque Volume and Obesity in Patients with Diabetes: The Factor-64 Study." which investigates the role of CT in measuring arterial plaque. It appears that computed tomography (CT) angiography imaging of the coronary arteries provides a precise evaluation of arterial plaque, potentially having a major impact on the management of diabetic patients facing an increased risk of cardiovascular events such as heart attacks.
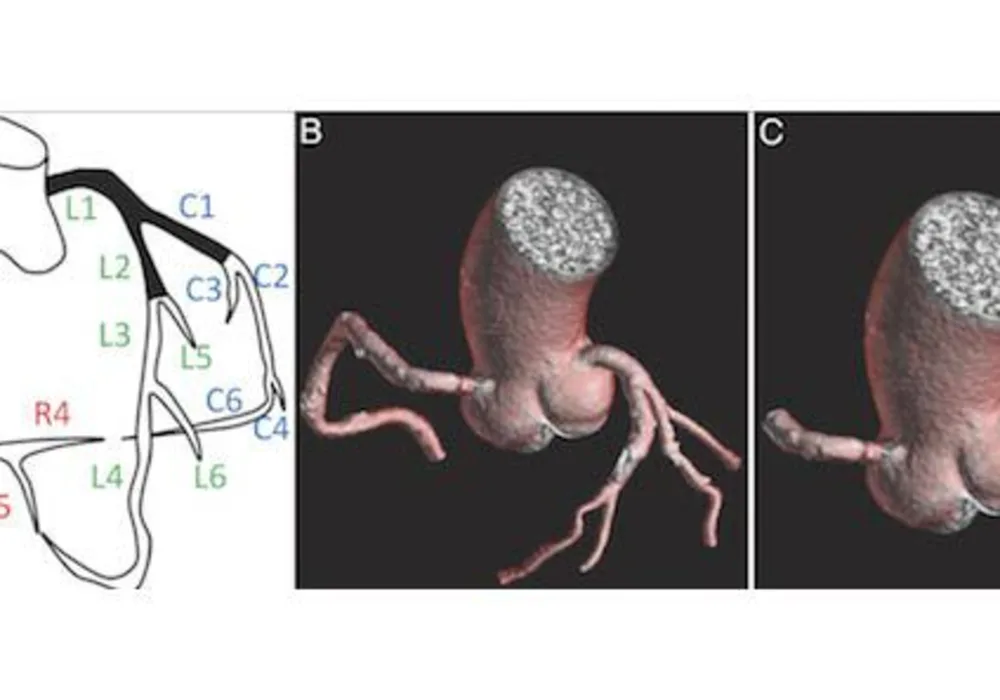
Figure 1 (main image). Coronary artery segment anatomy. A:Segmental nomenclature for coronary artery territories;B: Full segmentation of arteries more than 2 mm in diameter; C: Segmentation in same patient shows proximal segments C1, L1, L2, and R1.
Plaque, which forms in arterial walls, can lead to the restriction of blood flow and even rupture, causing possibly fatal heart attacks. Previous research has shown that plaque which is calcified, or stable, is less subject to rupture than non- calcified, or soft plaque. While it is possible to measure both types of coronary artery plaque via intravascular ultrasound, this method is invasive and inadequate for screening purposes. The common noninvasive alternative of coronary artery calcium (CAC) scoring with CT also has its limitations.
João A.C. Lima, MD, from the cardiology division at Johns Hopkins University in Baltimore, Maryland explains that despite showing the amount of calcified plaque present in a patient, calcium scoring is not capable of measuring the component that is not calcified, this is, however, the more dangerous one.
A viable screening option, the newly emerged quantitative plaque analysis with coronary computed tomography angiography (CCTA) can provide an instant, low radiation dose image of the coronary arteries’ entire anatomical map, offering an overview of the total amount of plaque across the heart’s arteries.
The multicenter study included researchers from the National Institutes of Health (NIH) in Bethesda, the Johns Hopkins, and the Intermountain Medical Center Heart Institute in Salt Lake City. The team conducted an evaluation of CCTA in close to 225 asymptomatic diabetic patients. Significant and untimely development of coronary artery plaque is prevalent in obese people with diabetes, which makes them an ideal study group for the assessment of plaque.
To establish a coronary plaque volume index (PVI) for each patient the team of researchers measured the coronary artery wall volume and length, providing them with far greater information than simply the presence or absence of coronary stenosis (narrowing). PVI was related to age, male gender, body mass index (BMI) and duration of diabetes, and younger individuals with a shorter duration of diabetes had a greater percentage of soft plaque.
As David A. Bluemke, MD, PhD, from the NIH Clinical Center pointed out, not only is coronary plaque volume index by CCTA clinically feasible and reproducible in diabetes patients, it further offers a more comprehensive picture of the coronary arteries that could be routinely applied in at-risk patients.
As assessed by CCTA, BMI - a measure of body fat based on weight and height - was the main variable risk factor linked to total and soft coronary plaque.
Dr. Bluemke stated that, since it was the only modifiable risk factor, obesity represented an important target for managing diabetic patients. He went on to stress the importance of evaluating BMI as a potential driver of overall diabetes.
Underscoring the widespread presence of non-calcified plaque, just one-third of the coronary plaque in patients showed calcification. Since treatment methods may vary based on plaque composition, it is vital to differentiate between calcified and non-calcified plaque.


Figure 2. Segmentation of left anterior descending artery with vascular model and coronary cross sections. Plaque subtypes are shown as follows: red = soft plaque, blue = fibrous plaque, yellow = calcified plaque. Green = luminal area. Note exclusion of ostia during segmentation. Plaque volume is the sum of all plaque component volumes.
Dr. Lima explained that patients with soft plaque responded better to interventions, in particular medical therapy like statins.
Dr. Lima explained that patients with soft plaque responded better to interventions, in particular medical therapy like statins.
With the aim of enhanced understanding of the value of coronary artery plaque assessment in predicting future cardiovascular events, and in order to further define the role of plaque volume index versus CAC score, the research team is set to carry on monitoring those patients who participated in the study.
To determine whether risk factor reduction would result in reduced PVI it would be necessary to conduct a clinical trial.
Noting that baseline indices of plaque in the study patients had been established, Dr. Bluemke added that the study could now focus on identifying those patients who, despite optimal management, experienced a cardiovascular disease event like a heart attack.
The researchers stated that CCTA was likely to be valuable for other groups of patients at high risk for cardiovascular events. They expressed hope that in future, this method would allow physicians to predict plaque development and treat it aggressively before PVI increases significantly.

Figure 3. Automated plaque detection. Red = soft plaque, blue = fibrous plaque, yellow = calcified plaque, green = luminal area. A: Image in patient with min¬imal plaque. B: Image in patient with large amounts of calcified plaque. C: Image in patient with both calcified plaque (upper left) and mixed plaque (lower right).
22 April 2014
Latest Articles
Imaging, RSNA, Heart, Angiography, arterial calcium, CT angiography, coronary, arterial plaque
The journal Radiology has published online the findings of a new multicenter study entitled "Coronary Artery Plaque Volume and Obesity in Patients with Dia...