Breast cancer is a significant global health concern, with over 2 million new cases diagnosed annually worldwide and nearly 8 million cases existing within a 5-year span. In Europe, it is the most prevalent cancer among women, comprising 15% of new cases overall and 30% among women specifically. Over half a million new cases are diagnosed annually in Europe alone, with approximately 13% of women facing a breast cancer diagnosis in their lifetime. While older women are more commonly affected, incidence rates have risen across all age groups globally in recent years, likely due to factors like increased screening programmes and changes in risk factors such as hormone exposure and smoking. Amidst advancements in diagnosis and treatment, the European Society of Breast Imaging (EUSOBI) recently published updated recommendations on breast cancer screening, while mortality remains a significant concern, with an estimated 140,000 deaths in Europe in 2020 and approximately 3% of women succumbing to the disease eventually.
Factors Influencing Breast Cancer Risk and Personalised Screening Strategies
Various factors contribute to an individual's risk of developing breast cancer, such as age at menarche and menopause, reproductive history, obesity, previous biopsy findings, radiation therapy, and family cancer history. Higher mammographic breast density also increases risk significantly. Risk prediction models, incorporating personal and genetic factors like BRCA mutations and mammographic density, aid in assessing individual risk, with deep learning models enhancing accuracy. Risk categories range from average to very high, based on lifetime risk percentages. High-risk individuals, especially those with genetic mutations like BRCA1/2, require specialised screening protocols starting from a young age. Ongoing trials explore personalised screening approaches based on individual risk assessment.
Advancements in Breast Cancer Screening and Evaluation of Effectiveness
Breast cancer screening aims to detect cancers at early, asymptomatic stages, enhancing chances of successful treatment. While breast self-examination was once advocated, it's now deemed ineffective in reducing mortality. Mammography, proven in randomised trials, allows early cancer detection, reducing breast cancer-related mortality by at least 20–25%. However, assessing screening's impact amid evolving treatments is complex. As evaluating new screening methods through mortality trials is unfeasible, surrogate endpoints like stage shift, interval cancer frequency reduction, and fewer advanced cancers are considered. These endpoints inform models of mortality reduction and cost-effectiveness.
Mammography
Mammography is the primary method for breast cancer screening, either through organized programs or opportunistic screening. In Europe, screening typically begins between ages 40-50 and continues until 64-74, with intervals of 1-2 years. High participation rates, recommended at 70-75%, are crucial for program effectiveness. Despite its benefits, mammography has limitations, especially in detecting cancers in women with dense breasts, where sensitivities drop significantly. Since dense breasts are common, comprising 40-50% of women, this poses a significant challenge. It's crucial to report breast density after mammography, as it informs decisions regarding supplemental or alternative imaging methods.
Digital Breast Tomosynthesis
Digital breast tomosynthesis (DBT) is an advanced imaging technique for breast cancer screening, involving multiple low-dose X-ray projections reconstructed into stacked images and a synthetic mammogram. DBT reduces the masking effect of overlapping breast tissue, improving cancer detection rates compared to mammography, with up to 4 additional cancers detected per 1000 screens. While DBT has decreased recall rates in high recall settings, European studies show similar or slightly higher recall rates. Despite its benefits, DBT's effectiveness is limited in women with very dense breasts, and concerns about overdiagnosis persist due to increased detection of slow-growing tumours. Studies on DBT's impact on interval cancer rates yield mixed results. Synthetic mammography, derived from DBT datasets, serves as an alternative to traditional mammography, maintaining screening performance while reducing radiation exposure and image acquisition time.
Breast Ultrasound
Supplemental breast ultrasound screening in women with dense breasts enhances cancer detection rates by 0.9–7.7 per 1000 screenings and reduces interval cancer rates compared to mammography alone. Automated breast ultrasound systems mitigate the limitations of handheld ultrasound but may increase recall and biopsy rates, reducing the positive predictive value of screening to about 5%. Despite its benefits, concerns about cost-effectiveness persist due to long examination times. While guidelines suggest considering supplemental ultrasound for women with dense breasts and negative mammograms, the overall balance of advantages and disadvantages isn't deemed clear enough for widespread adoption.
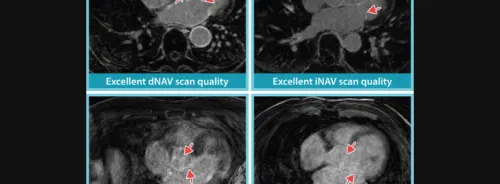
MRI
Breast MRI stands out as the most sensitive imaging method for breast cancer detection, particularly effective due to its ability to detect neovascularity and target aggressive tumour subtypes. Unlike mammography, breast density doesn't limit MRI sensitivity. Yearly MRI screening is recommended for women with genetics-based increased risk or history of chest radiation. Supplemental mammography may be considered for women aged 35–40. Recent trials support MRI screening for women with extremely dense breasts, offering cost-effective mortality reduction. Challenges include higher costs, limited availability needing expansion, and long examination times, though abbreviated protocols show promise in addressing the latter.
Contrast-Enhanced Mammography
Contrast-enhanced Mammography (CEM) is a novel breast imaging technique utilizing contrast medium, akin to breast MRI, to visualize vascularity linked to breast cancer, offering both anatomical and functional insights simultaneously. While few studies have explored CEM in screening, especially among women with intermediate/high lifetime risk, it exhibits superior diagnostic performance compared to digital mammography, DBT, and mammography with supplemental ultrasound, with comparable or slightly higher specificity but lower sensitivity than breast MRI. Consequently, CEM emerges as a promising alternative to breast MRI in settings where MRI isn't available. However, most current studies are retrospective or involve a limited number of participants, necessitating larger-scale investigations to compare CEM with standard imaging modalities, particularly MRI, regarding stage shift achieved and frequency of interval and advanced cancers.
Downsides and Risks Associated with Screening
Mammography screening for breast cancer offers proven benefits in reducing mortality rates, but it also comes with significant drawbacks that must be considered. Underdiagnosis is a concerning issue where clinically relevant breast cancer may be present but goes undetected during screening. This can lead to delayed detection, allowing cancer to progress and become less treatable over time. Studies suggest that a significant portion of cancers detected through mammography are already visible on previous mammograms but were not recognised at the time. Underdiagnosis rates vary, ranging from 15-40% depending on factors like breast density. Other screening modalities, such as breast MRI, have shown potential in detecting cancers earlier, but predicting cancer type remains challenging.
False positive results are another challenge, affecting up to 10-12% of screened women. This can lead to unnecessary anxiety, additional medical procedures like biopsies, and increased healthcare costs. European guidelines recommend double reading of mammograms to reduce false positives, as it has been shown to maintain cancer detection rates while lowering recall rates. False positives can also deter women from participating in future screenings due to anxiety or discomfort.
Overdiagnosis is a complex issue where cancers are detected that would never cause harm if left untreated. These slower-growing, lower-grade cancers are more likely to be identified through mammography screening, leading to unnecessary treatments that may cause harm without providing benefits. Estimating the extent of overdiagnosis is challenging, with studies reporting percentages ranging from 0-50% of all detected cancers. Identifying women with low-risk disease may help reduce overtreatment, and ongoing trials are exploring active monitoring as an alternative to surgery for certain cases of ductal carcinoma in situ.
Economic Considerations and Patient Preferences
Breast cancer screening's cost-effectiveness varies based on local factors such as imaging costs, labour, and the value placed on improved life expectancy and overall health. Economic models indicate that in European healthcare settings, screening improves life expectancy and quality-adjusted life expectancy at acceptable costs. Risk-adapted screening strategies can optimise resource use by tailoring screening methods to each risk category, reducing unnecessary harm and costs. In resource-limited countries, screening tools should be chosen based on cost-effectiveness and performance. When large-scale screening isn't feasible due to financial constraints, priority should be given to raising awareness about breast cancer and ensuring timely presentation of breast complaints to radiologists, potentially through education on physical breast examination and modifiable risk factors.
Women should receive comprehensive information about both the benefits and drawbacks of screening tests to enable informed decision-making. Providing prompt screening results helps minimise anxiety. Shared decision-making, involving both physicians and patients, ensures that decisions are based on scientific evidence as well as individual expectations and preferences. Breast radiologists play a crucial role in this process due to their specialised knowledge. While many women prioritise early diagnosis, concerns about overdiagnosis and false positives persist, highlighting the need for a better understanding of these concepts. As screening approaches become more tailored to individual risk levels, informed decision-making becomes even more critical, particularly for women eligible for reduced screening intensity.
EUSOBI’s Breast Cancer Screening Recommendations
Screening mammography is a highly effective tool in reducing breast cancer mortality, supported by strong evidence (level I). It is recommended that existing screening programmes continue, with a focus on increasing adherence to ensure maximum benefit. Additionally, digital breast tomosynthesis can serve as an alternative to traditional mammography, offering improved imaging capabilities.
For high-risk women, screening should begin as early as 25 years of age, with annual breast MRI recommended (also evidence level I), supplemented by mammography starting between ages 35 to 40. This approach aims to detect potential cancers at the earliest stages, improving treatment outcomes.
Women at intermediate risk of breast cancer may benefit from supplemental screening methods, including digital breast tomosynthesis, breast ultrasound, breast MRI, and possibly contrast-enhanced mammography (CEM). The selection of the most appropriate imaging modality should be based on individual patient characteristics to maximise effectiveness.
The current evidence strongly supports the use of breast MRI screening every 2-3 years for women with extremely dense breast tissue. In cases where MRI is not available, supplemental ultrasound can be considered as an alternative, although its added value in terms of cancer detection may be more limited.
Various risk prediction models are available to estimate individual breast cancer risk. It is recommended to initiate risk assessment at a younger age, around 25 years old, to effectively tailor screening recommendations to each woman's specific risk profile.
Ultimately, screening decisions should involve shared decision-making between women and their healthcare providers. This collaborative approach ensures that screening recommendations align with each woman's preferences, values, and individual circumstances, optimising the effectiveness of breast cancer screening efforts.
Source: European Radiology
Image Credit: iStock