The COVID-19 pandemic has accelerated the adoption of remote healthcare pathways worldwide, moving away from traditional face-to-face models. This shift includes integrating telemedicine and remote monitoring solutions, which offer advantages such as reducing viral exposure risk and providing quality care remotely. The concept of "virtual wards" allows selected individuals to receive care at home rather than in secondary care facilities. Despite the potential benefits, implementing digital technologies in complex hospital systems faces challenges, including a lack of standardised procedures and evaluation methods. For instance, a study in the UK's National Health Service (NHS) found that although wearable sensors could detect clinical deterioration, response times to alerts were delayed. Patient acceptance of such digital tools is generally high, but concerns exist around overreliance on data and reduced contact with clinical staff. Healthcare staff perceptions vary, with concerns about increased workloads and the clinical significance of collected data. NHS initiatives, supported by organisations like NHS Digital, aim to drive digital transformation in health care, including the development of virtual wards. To effectively implement remote monitoring solutions, understanding organisational barriers and facilitators is crucial. A proposed framework, HOT-fit, evaluates alignment among humans, organisations, and technology, offering a structured approach to enhance the success of digital healthcare initiatives. A recent study published in JMIR Human Factors aimed to assess stakeholder perspectives within the NHS and identify factors affecting successful implementation of remote monitoring solutions, ultimately proposing a roadmap for integrating wearable solutions in secondary care.
Exploring the Methodological Frameworks
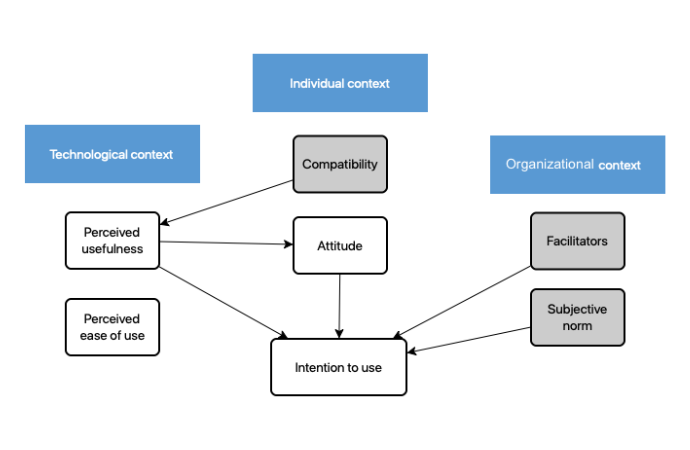
A mixed methods approach was used, combining semistructured interviews and questionnaires, following recommendations from the Standards for Reporting Qualitative Research (SRQR) guidelines. Semistructured interviews involved high-level stakeholders from industry, academia, and health care providers with experience in implementing digital solutions. Recruitment followed a key informant strategy, targeting individuals with notable contributions to remote monitoring solutions in health care. A validated questionnaire, based on the Technology Acceptance Model (TAM), was employed to assess technological acceptance. The theoretical framework integrated individual, technological, and organisational contexts, focusing on factors like compatibility, perceived usefulness, and subjective norms. Interviews were guided by a structured topic guide and recorded for analysis using NVivo software. The iterative data collection process allowed for exploration of emerging concepts, ensuring comprehensive analysis of stakeholder perspectives.
Identifying Facilitators and Challenges
One significant facilitator identified was the improvement of workflow efficiency. Stakeholders emphasised the importance of streamlining processes to integrate digital solutions seamlessly into existing clinical workflows. Additionally, providing adequate troubleshooting support for staff was highlighted as essential to address technical challenges and ensure smooth operation of the digital tools. Engaging positively with health care staff emerged as another crucial facilitator. Stakeholders emphasised the importance of fostering a supportive and collaborative environment to encourage staff acceptance and participation in the implementation process. Identifying and involving local champions within the clinical workforce was suggested as an effective strategy to promote engagement and facilitate integration.
Addressing Implementation Challenges
However, the study also revealed various challenges associated with implementing remote monitoring solutions. Poor training was identified as a significant barrier, hindering staff proficiency in utilizing the digital tools effectively. Additionally, stakeholders expressed concerns about the burden of data, particularly with continuous remote monitoring of vital signs. Issues such as the clinical meaningfulness of the collected data and inadequate resourcing further compounded the challenges faced by staff. Despite these challenges, stakeholders recognized the potential benefits of remote monitoring technology in improving patient care and clinical outcomes. Perceived usefulness and ease of use were identified as critical factors influencing the acceptance and adoption of these digital tools. Stakeholders emphasized the importance of intuitive and user-friendly systems to facilitate successful implementation and utilization.
The study underscored the complexity of integrating digital solutions into clinical practice within the NHS. While there are significant opportunities to enhance patient care through remote monitoring technology, addressing the identified barriers and leveraging the facilitators will be crucial to realizing its full potential. By prioritizing staff engagement, providing adequate training and support, and ensuring the usability of digital tools, health care organizations can overcome implementation challenges and effectively integrate remote monitoring solutions into routine clinical workflows.
Source & Image Credit: JMIR Human Factors






