The Executive Board of the German Society for Anesthesiology recently adopted a new guideline that addresses the intraoperative clinical application of hemodynamic monitoring in non-cardiac surgical patients.1
Why continuous hemodynamic monitoring?
The aim of this special guideline was to identify the questions that are important for daily clinical practice and to answer them based on current evidence. Hemodynamic monitoring and management ensure perioperative monitoring and therapy of cardiovascular function and form the basic pillars of perioperative anesthesiological treatment to maintain organ functions. Furthermore, perioperative complications should be avoided, the rate of which is still very high at almost 20% 1. Long-term morbidity with an influence on mortality and quality of life is very often the result.
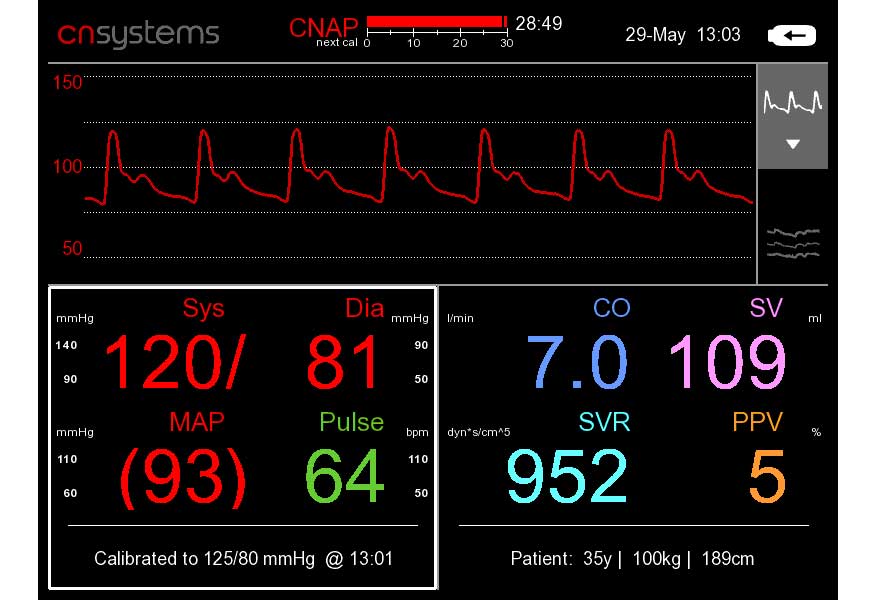
Continuous blood pressure measurement enables the detection and thus immediate therapy of rapidly occurring hypotension or hypertension. Continuous blood pressure measurement can therefore help to reduce the occurrence of blood pressure fluctuations and intraoperative hypotension.
The assessment of volume responsiveness is an important component in volume therapy. Volume responsiveness means that the stroke volume/cardiac output can be increased by a fluid bolus. The test procedures are used to assess volume responsiveness after considering the clinical situation and taking into account the inherent limitations of the procedure. Basically, it is important to avoid both volume deficiency and volume overload.
Recommendations of the guidelines expert group for continuous monitoring
However, the individual components of hemodynamic monitoring can only represent partial aspects of the overall evaluation of the patient’s clinical situation. The monitoring methods are therefore differentiated depending on the patient’s condition in the context of his anamnesis and preliminary examinations. The spectrum ranges from non-invasive basic monitoring, which can be used in all patients, to the use of the pulmonary artery catheter in highly selected patients. According to the guidelines group, interdisciplinary communication is also essential here.
With regard to the intraoperative monitoring of hemodynamic values, in particular blood pressure, stroke and cardiac output, as well as dynamic fluid parameters, the new guideline contains the following recommendations:
- Continuous arterial blood pressure monitoring should be carried out in all patients who are at risk of complications such as hypo- or hypertension.
- Continuous measurements can be measured invasively or non-invasively (e.g. via a finger sensor), depending on the patient’s clinical condition and history.
- In appropriate patients, e.g. low or intermediate risk, non-invasive continuous blood pressure monitoring may be considered.
- Continuous measurement of hemodynamic values should in principle be the preferred method over intermittent measurement.
- Stroke volume and cardiac output monitoring can be used in patients during surgery.
- Dynamic preload parameters (e.g. pulse pressure variation PPV or stroke volume variation SVV) should be used to evaluate volume responsiveness in controlled ventilated patients.
- If possible, the raw signals of the measurement should be displayed in addition to the numerical values of the hemodynamic measurement in order to detect artifacts and derive further diagnostic information.
- Reducing or avoiding invasive hemodynamic monitoring should be the goal to improve the risk-benefit ratio.
The advantages of non-invasive technologies
The technical options for cardiovascular monitoring have developed significantly in recent years; less invasive and non-invasive measurement methods are on the market, which can contribute to better treatment results in the long term as they significantly reduce risk and complications.
The findings of further studies by the team of authors from Hamburg also fall into this line. Non-invasive finger sensors enable continuous monitoring of blood pressure without having to insert an arterial catheter. Continuous monitoring during anesthesia induction and during surgery reduces hypotension compared to the intermittent blood pressure measurement method.
Recent studies favor non-invasive continuous monitoring

Continuous monitoring of arterial blood pressure using a finger cuff during non-cardiac procedures helps to effectively reduce hypotension within the first 15 minutes after the start of anesthesia and thus prevent more serious drops in blood pressure.4 Again, the recommendation of the experts is as follows: “Clinicians might reasonably consider continuous finger cuff monitoring in patients who would otherwise be monitored with intermittent oscillometric monitoring.”4
Apart from the reduced risk due to the better recognition of hypotonic episodes, the agreement between finger blood pressure measurement and intra-arterial measurement is far better than between oscillometric blood pressure measurement and intra-arterial catheter measurement. „Continuous monitoring of blood pressure is an intriguing new concept that has the potential to revolutionize patient care.”3
The study by Gore et al. goes one step further and addresses the question of whether non-invasive technologies for continuous blood pressure measurement have the potential to replace invasive measurements. The conclusions show that although we will certainly not eliminate arterial measurement for critically ill patients, we see promising fields of application for non-invasive blood pressure monitors:
“In the future, non-invasive continuous BP monitors will likely replace intermittent oscillometers in the operating room and the postoperative period.”4

Source & Image: CNSystems
References:
1 Saugel B, et al. S1-Leitlinie Intraoperative klinische Anwendung von hamodynamischem Monitoring bei nicht-kardiochirurgischen Patient:innen, available here
2 Bergholz, A., Greiwe, G., Kouz, K. & Saugel, B. Continuous Blood Pressure Monitoring in Patients Having Surgery: A Narrative Review. Medicina (Kaunas). 59, 1–10 (2023). View abstract
3 Kouz, K. et al. Continuous finger-cuff versus intermittent oscillometric arterial pressure monitoring and hypotension during induction of anesthesia and non-cardiac surgery: The DETECT randomized trial. Anesthesiology (2023). doi:10.1097/ALN.0000000000004629. View abstract
4 Gore P, Liu H, Bohringer C (February 22, 2024) Can Currently Available Non-invasive Continuous Blood Pressure Monitors Replace Invasive Measurement With an Arterial Catheter? . Cureus 16(2): e54707. DOI 10.7759/cureus.54707. View abstract