ICU Management & Practice, Volume 24 - Issue 3, 2024
We discuss the economic and environmental advantages of green pulse wave analysis (PWA) techniques and the integration of PWA algorithms into standard bedside monitors that will likely contribute to democratisation of perioperative cardiac output monitoring.
Haemodynamic instability frequently manifests during the perioperative course of high-risk surgical patients. This instability arises primarily during surgery due to the influence of anaesthetic agents on sympathetic activity and vascular tone, compounded by surgical bleeding. Post-surgery, various factors may be responsible for haemodynamic instability, including haemorrhagic complications, cardio-respiratory adverse events (such as myocardial infarction and pulmonary embolism), and infectious complications (e.g. septic shock). Haemodynamic instability can precipitate tissue hypoperfusion and hypoxia and, if prolonged, may culminate in organ failure, ultimately leading to postoperative mortality. In this context, rational haemodynamic management requires quantifying cardiac output (CO) and vascular tone to identify the underlying mechanisms of haemodynamic instability and select the right treatment (Figure 1).

The Evolution of Haemodynamic Monitoring Tools
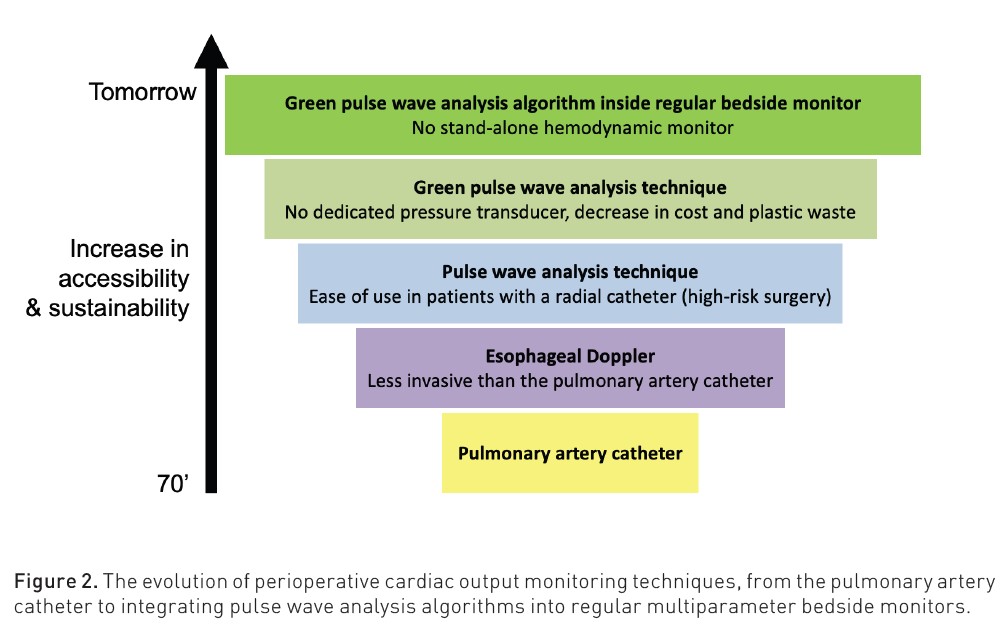
In the 70s, the introduction of the (yellow) pulmonary artery catheter allowed clinicians to better characterise haemodynamic profiles than with heart rate and blood pressure only. Both hypovolaemic and vasodilatory states, common during general anaesthesia and surgery, became easy to identify. Indeed, hypovolaemia is characterised by a decrease in cardiac filling pressures and blood flow (stroke volume and CO), whereas vasodilation is characterised by a decrease in systemic vascular resistance.
In the 90s, the development of less invasive and quicker-to-set-up oesophageal Doppler techniques led to the progressive decline of pulmonary artery catheter use during major surgical procedures (Wiener et al. 2007), with a few notable exceptions that include cardiac surgery (monitoring and manipulating pulmonary artery pressures may be useful in patients with right ventricular failure) and liver transplantation. Several studies have reported patient outcome benefits when using the oesophageal Doppler technique to guide perioperative haemodynamic management (Gan et al. 2002).
At the beginning of the 21st century, perioperative haemodynamic monitoring was further simplified by the inception of the arterial pulse pressure variation (PPV). This variable predicts fluid responsiveness without the need to track CO changes during a preload-modifying manoeuvre (e.g. a fluid challenge or a passive leg-raising manoeuvre) (Michard 2005). Several studies have reported patient outcome benefits when using PPV to guide intraoperative haemodynamic management (Benes et al. 2014). However, PPV cannot be used in all circumstances. During surgery with general anaesthesia, the main limitations to the use of PPV are laparoscopic surgery (increased abdominal pressure), thoracic surgery (open chest), and cardiac arrhythmia (mainly atrial fibrillation). Of note, a tidal volume of 7-9 ml/kg, commonly used during surgery and deemed safe (Levin et al. 2015), is compatible with the use of PPV.
Pulse wave analysis (PWA) algorithms compute stroke volume and CO from the arterial pressure waveform (Chew et al. 2013). They allow clinicians to assess blood flow and vascular tone (total vascular resistance = mean arterial pressure divided by CO) in all patients who have a radial catheter in place for continuous blood pressure monitoring. Many studies have reported patient outcome benefits when using PWA techniques to guide perioperative haemodynamic management (Michard et al. 2017). The first PWA technique that did not require external calibration (with thermodilution or lithium dilution) was launched in 2005. Since then, multiple PWA techniques have become available. In a large European study done in 28 countries, 73% of anaesthesiologists who monitored CO during surgery did so with a PWA technique (Ahmad et al. 2015). This proportion increased to 92% in a recent European survey (Flick et al. 2023). Put differently, contemporary anaesthesiologists overwhelmingly favour PWA techniques as their primary method for monitoring CO (Figure 2).
How to Improve the Accessibility and Sustainability of PWA Techniques
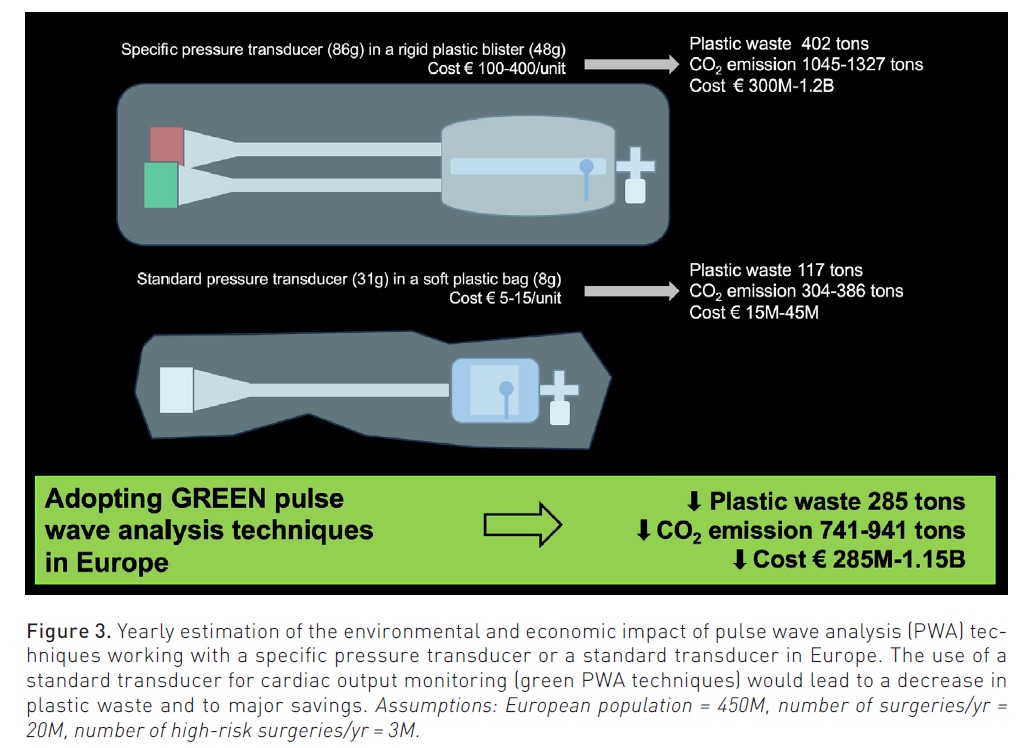
Despite the development of PWA techniques, only 10 to 40% of surgical patients undergoing high-risk surgery have their CO monitored during the procedure (Molliex et al. 2019; Flick et al. 2023). According to a recent European survey, the main barrier to the clinical adoption of CO monitoring systems is their availability and cost (Flick et al. 2023). Addressing this financial challenge is pivotal to ensuring equitable access to advanced monitoring technologies and unlocking the full potential of PWA techniques. Recently, a nationwide French study (Michard et al. 2023) assessed the costs of using PWA techniques that work either with a dedicated pressure transducer or with any standard pressure transducer. Because of the significant cost difference between dedicated and standard pressure transducers (€150/transducer in the French participating centres), adopting standard pressure transducers for CO monitoring would reduce hospital costs by €67 million/yr. In France, this is the budget necessary to hire >2,000 nurses or to buy >10,000 pocket ultrasound devices each year. If, as recommended by the French Society of Anesthesiology and Intensive Care (SFAR), all high-risk surgical patients had their CO monitored (https://lnkd.in/esZkzZBe), the cost reduction would reach €187 million/yr. When extrapolating these findings to the European population and considering some specific pressure transducers may cost up to €300-400/unit, savings could exceed €1 billion/yr (Figure 3).
The climate crisis poses another significant challenge, prompting hospitals to actively seek solutions for reducing their carbon footprint. A growing trend is anticipated in the adoption of solutions that minimise plastic waste and mitigate carbon dioxide emissions (Davies et al. 2023). The above-mentioned nationwide French study (Michard et al. 2023) also compared the carbon footprint of PWA techniques requiring a dedicated pressure transducer to those working with any standard pressure transducer. Given the plastic weight difference between dedicated and standard pressure transducers, prioritising the use of standard transducers for CO monitoring would reduce plastic waste by 25 tons/yr and carbon dioxide emissions between 65 and 83 tons/yr. If the SFAR recommendations were followed, the reduction in carbon dioxide emissions would reach 179-227 tons/yr. When considering the additional packaging-related plastic waste (rigid plastic blister for dedicated pressure transducer vs soft plastic bag for standard pressure transducer) and extrapolating to the European population, the reduction would be close to 1000 tons of carbon dioxide (Figure 3). Thus, PWA techniques working with any standard pressure transducer, now known as “green” PWA techniques, are a preferable option both from an economic and environmental standpoint.
Whether green PWA techniques are as reliable as other PWA techniques is a legitimate question. Multiple studies have compared both green and other PWA techniques to reference CO measurements (by thermodilution or echocardiography) and have yielded conflicting results, depending on the patient population and the clinical situation. Only a limited number of clinical studies have compared several PWA techniques to a reference method in the same patients at the same time. Two studies (Hadian et al. 2010; Lamia et al. 2018) compared the LiDCOrapid and the FloTrac algorithms to reference pulmonary thermodilution in postoperative cardiac surgery patients. The lowest bias, the narrowest limits of agreement, and the best concordance rates to track changes in thermodilution CO were observed with the LiDCOrapid algorithm. Another study (Romagnoli et al. 2013) compared the MostCareUp and the FloTrac algorithms to reference echocardiography in patients undergoing vascular surgery. This study reported a better precision (i.e. a lower percentage error) with the MostCareUp algorithm. Interestingly, both the MostCareUp and LiDCOrapid are green PWA techniques. Thus, head-to-head comparison studies published so far support the notion that favouring the use of green monitoring solutions will not be to the detriment of accuracy and precision.
Conclusion and Perspectives
Perioperative haemodynamic monitoring tools have undergone remarkable transformations over the past five decades, progressing from yellow pulmonary catheters to contemporary green PWA techniques. In patients with a radial arterial catheter, PWA techniques have the advantage of instantly providing non-operator-dependent and continuous information about blood flow and vascular tone. Green PWA techniques not only reduce plastic waste but also contribute to significant cost savings in hospital expenditures, making them a recommendable solution.
Anticipating future developments, PWA algorithms are poised to integrate seamlessly into multiparameter bedside monitors, obviating the need for standalone haemodynamic monitors and further decreasing the cost and carbon footprint of haemodynamic monitoring. The forthcoming democratisation of CO monitoring holds the promise of empowering a growing number of clinicians to make timely and informed therapeutic decisions, ensuring a greater proportion of high-risk surgical patients benefit from advanced haemodynamic management.
Conflict of Interest
Frederic Michard is the founder and managing director of MiCo, a consulting and research firm based in Switzerland. Michelle Chew is the chair of the ESICM cardiovascular dynamics section. Pierre-Grégoire Guinot received fees for lectures from Baxter, Edwards, and Vygon.
References:
Ahmad T, Beilstein CM, Aldecoa C et al. (2015) Variation in haemodynamic monitoring for major surgery in European nations: secondary analysis of the EuSOS dataset. Perioper Med. 4:8.
Benes J, Giglio MT, Brienza N, Michard F (2014) The effects of goal-directed fluid therapy based on dynamic parameters on post-surgical outcome: a meta-analysis of randomized controlled trials. Crit Care. 18:584.
Chew MS, Aneman A (2013) Haemodynamic monitoring using arterial waveform analysis. Curr Opin Crit Care. 19:234-41.
Davies JF, Ikin B, Francis JJ, McCain F (2023) Implementation approaches to improve environmental sustainability in operating theatres: a systematic review. Br J Anaesth. Online ahead of print.
Flick M, Joosten A, Scheeren T et al. (2023) Haemodynamic monitoring and management in patients having non-cardiac surgery. A survey among members of the European Society of Anaesthesia and Intensive Care. Eur J Anaesth Intensive Care. 1:pe0017.
Gan TJ, Soppitt A, Maroof M et al. (2002) Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology. 97: 820-6.
Hadian M, Kim HK, Severyn DA, Pinsky MR (2010) Cross-comparison of cardiac output trending accuracy of LiDCO, PiCCO, FloTrac and pulmonary artery catheters. Crit Care. 14:R212.
Lamia B, Kim HK, Severyn DA, Pinsky MR (2018) Cross-comparisons of trending accuracies of continuous cardiac output measurements. J Clin Monit Comput. 32.33-43.
Levin MA, McCormick PJ, Lin HM et al. Low intraoperative tidal volume ventilation with minimal PEEP is associated with increased mortality. Br J Anaesth. 113:97-108.
Michard F (2005) Changes in arterial pressure during mechanical ventilation. Anesthesiology. 103:419-428.
Michard F, Futier E, Desebbe O et al. (2023) Pulse contour techniques for perioperative hemodynamic monitoring: A nationwide carbon footprint and cost estimation. Anaesth Crit Care Pain Med. 42:101239.
Michard F, Giglio MT, Brienza N (2017) Perioperative goal-directed therapy with uncalibrated pulse contour methods: impact on fluid management and postoperative outcome. Br J Anaesth. 119:22-30.
Molliex S, Passot S, Morel J et al. (2019) A multicentre observational study on management of general anaesthesia in elderly patients at high-risk of postoperative adverse outcomes. Anaesth Crit Care Pain Med. 38:15-23.
Romagnoli S, Ricci Z, Romano SM et al. (2013) FloTrac/Vigileo (third generation) and MostCare/PRAM versus echocardiography for cardiac output estimation in vascular surgery. J Cardiothorac Vasc Anesth. 27:1114–1121.
Wiener RS, Welch HG (2007) Trends in the use of the pulmonary artery catheter in the United States, 1993-2004. JAMA. 298:423-429.