In locally advanced pancreatic cancer (LAPC), preventing local progression is crucial as it significantly impacts survival rates. Intraoperative radiotherapy (IORT) has shown promise in improving local disease control rates. However, determining the risk of progression in patients initially assessed as stable disease (SD) after IORT remains challenging. Efforts, including clinical, molecular, and imaging approaches, have been made to stratify this risk, but further investigation is needed. Multi-detector computed tomography (MDCT) is recommended for evaluating pancreatic cancer, with the extracellular volume (ECV) fraction derived from contrast-enhanced CT (CECT) showing potential as an imaging biomarker for predicting tumour aggressiveness and treatment response. ECV reflects pancreatic fibrosis, which plays a role in tumour progression and chemoresistance. However, current methods for estimating ECV are time-consuming or require specialised equipment.
A recent study published in Insights into Imaging aimed to assess whether ECV derived from the portal-venous phase (PVP) of conventional CT could serve as a non-invasive imaging biomarker for predicting progression in LAPC patients initially assessed as SD after IORT. Additionally, the study aimed to construct a risk-scoring system based on ECV and clinical-radiological features to evaluate progression risk in these patients.
Study Overview: Analysing ECV and Developing a Risk-Scoring System
In a retrospective study approved by the institutional review board, 103 patients with locally advanced pancreatic cancer (LAPC) who received intraoperative radiotherapy (IORT) and demonstrated stable disease (SD) on imaging were analysed. Patients underwent multiphasic contrast-enhanced CT (CECT) before and after IORT. ECV maps were generated from unenhanced and portal-venous phase (PVP) CT images. Among the initially enrolled 184 patients, 81 were excluded, resulting in a final cohort of 103 patients (64 males, 39 females; mean age 58.52 ± 10.09 years). All patients underwent standard multi-phase CECT scans, including non-enhanced (N), arterial phase (AP), pancreatic parenchymal phase (PPP), and PVP. Iopromide was administered at a rate of 3.5 mL/sec, with a weight-dependent dose of 1.5 mL/kg. The average delay times for AP, PPP, and PVP were 25–30 s, 40–50 s, and 65–70 s, respectively. Multiple CT scanners were used due to the retrospective nature of the study.
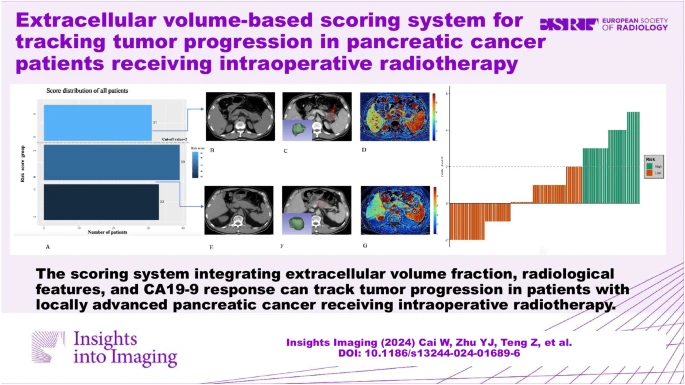
Image Credit: Insights into Imaging
ECV as an Independent Predictor and Development of the Risk-Scoring System
The analysis revealed that the ECV fraction derived from PVP was independently associated with the risk of progression in LAPC patients with SD post-IORT. Additionally, a novel risk-scoring system was developed, integrating ECV, CT radiological features (such as rim enhancement and peripancreatic fat infiltration), and CA19-9 response. CA19-9 response refers to the change in CA19-9 levels after treatment, which is an indicator of treatment efficacy and prognosis in pancreatic cancer.
The study found that patients with a high ECV value from PVP had a lower risk of progression, likely due to factors such as tumour stroma composition, vascular deficiency, and tissue hypoxia. Furthermore, CT radiological features such as rim enhancement and peripancreatic fat infiltration were identified as consistent predictors of LAPC progression.
Understanding the Mechanisms: ECV, CT Radiological Features, and CA19-9 Response
CA19-9 response also contributed significantly to the scoring system's predictive accuracy. Patients who showed a significant decrease in CA19-9 levels after treatment had a longer progression-free survival (PFS) compared to those who did not. However, the study had some limitations, including its retrospective design, relatively small sample size, and single-institution data. Moreover, the consistency between PVP-based ECV and equilibrium-based ECV was not investigated, and further research is needed to validate the findings prospectively.
ECV derived from PVP can be used to predict the progression risk in LAPC patients initially assessed as SD after IORT. The risk-scoring system integrating ECV, CT radiological features, and CA19-9 response could be an efficient and practical tool for prognosis stratification in LAPC patients with SD. It could assist RECIST v.1.1 to further identify SD patients who might be sensitive to and benefit from IORT accurately, aiding clinicians in choosing individual treatment strategies, preventing tumour progression, and improving the prognosis of patients with LAPC after IORT.
Source: Insights into Imaging
Image Credit:iStock