Oesophageal cancer (EC) is a growing concern globally, with multidisciplinary treatments offering the best chance of cure. However, despite advancements, the 5-year survival rate remains low. Accurate staging is crucial for treatment decisions, but current methods like endoscopic ultrasound (EUS) have limitations, leading to overestimation of tumour depth and poor nodal staging. Complementary imaging techniques like CT, MRI, and PET have been used, but their sensitivity and specificity are still limited. Radiomics, which extracts quantitative features from images, shows promise in predicting TNM stages, with CT, MRI, and PET-based radiomics demonstrating varying levels of accuracy. PET-CT radiomics has also been applied successfully to predict outcomes post-treatment. While pathological staging is the most precise, preoperative prediction using radiomics could greatly aid decision-making. Thus, a study published in Insights into Imaging aimed to explore the accuracy of radiomics from CT, PET, and PET-CT in predicting both clinical and pathological stages for EC patients.
Methodology: Retrospective Analysis of Patients and Imaging Techniques
In this retrospective study, patients diagnosed with oesophageal cancer (EC) from January 2011 to December 2020 were analysed. The study involved searching electronic medical records at the author's hospital. All enrolled patients had confirmed EC through pathology and underwent 18F-FDG PET-CT within one month before surgery, without prior radiotherapy or chemotherapy. TNM stages were determined by an experienced radiation oncologist according to the AJCC eighth edition TNM staging guidelines, utilising postoperative pathology results. Exclusions were made for patients without preoperative PET-CT, missing images, incomplete pathology data, non-squamous cell carcinoma (SCC) pathology, or treatments other than surgery. The hospital's Ethics Committee in Clinical Research approved the study, adhering to the Helsinki Declaration.
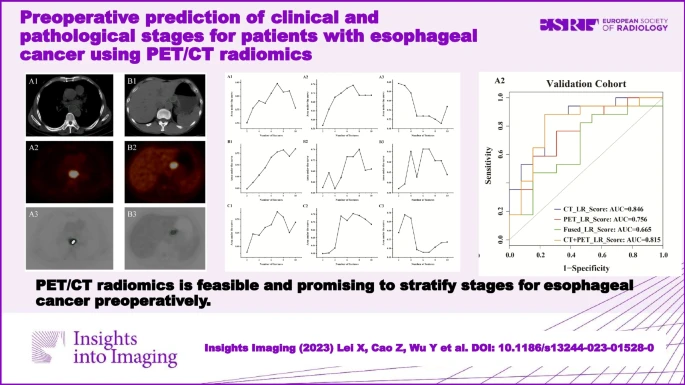
Histologically confirmed, 100 EC patients with preoperative PET-CT images were enrolled retrospectively and randomly divided into training and validation cohorts at a ratio of 7:3. The maximum relevance minimum redundancy (mRMR) was applied to select optimal radiomics features from PET, CT, and fused PET-CT images, respectively. Logistic regression (LR) was applied to classify the T stage (T1,2 vs. T3,4), lymph node metastasis (LNM) (LNM(−) vs. LNM(+)), and pathological state (pstage) (I–II vs. III–IV) with features from CT (CT_LR_Score), PET (PET_LR_Score), fused PET/CT (Fused_LR_Score), and combined CT and PET features (CT + PET_LR_Score), respectively.
Seven, 10, and 7 CT features; 7, 8, and 7 PET features; and 3, 6, and 3 fused PET/CT features were selected using mRMR to predict T stage, LNM, and pstage, respectively. The area under curves (AUCs) for T stage, LNM, and pstage prediction in the validation cohorts were 0.846, 0.756, 0.665, and 0.815; 0.769, 0.760, 0.665, and 0.824; and 0.727, 0.785, 0.689, and 0.837 for models of CT_LR_Score, PET_ LR_Score, Fused_ LR_Score, and CT + PET_ LR_Score, respectively.
Source: Insights into Imaging
Evaluation of Radiomics Models for T Stage, LNM, and Pstage Prediction
The combined CT and PET radiomics model (CT + PET_LR_Score) showed the best performance for predicting N stage and pathological stage (pstage), with AUCs of 0.824 and 0.837 in the validation cohort, respectively. For T stage prediction, the CT radiomics model (CT_LR_Score) demonstrated an AUC of 0.871 in the training cohort and 0.846 in the validation cohort. Despite advances in imaging, single noninvasive modalities still have limitations in accurately determining clinical staging. CT, commonly used for nodal staging, demonstrated relatively low sensitivity (54.5%) and moderate accuracy. Radiomics from CT alone achieved an accuracy of 73.3% for predicting lymph node metastasis (LNM) in the validation cohort. However, combining CT and PET radiomics resulted in lower accuracy for LNM prediction, possibly due to increased feature dimensionality.
Performance Comparison of Imaging Modalities and Limitations of Current Methods
Endoscopic ultrasound (EUS) is often used for T staging but is affected by oesophageal stenosis, leading to reduced accuracy. In this study, radiomics models using CT alone or combined CT and PET showed improved accuracy in T stage prediction compared to EUS. PET-CT is valuable in non-invasively determining stage status, with studies showing high accuracy when combined with parameters like maximum SUV (SUVmax). However, in this study, the LR model based on CT alone radiomics performed better than combined CT and PET radiomics or PET alone radiomics for T stage prediction. PET-CT radiomics had the lowest performance, possibly due to the loss of tumour information in fused images. Limitations of the study include the exclusion of patients receiving preoperative chemoradiotherapy, the lack of investigation into clinical risk factors, and the relatively small sample size from a single centre. Further studies with larger cohorts and external validation are needed.
In this study, combined PET and CT radiomics accurately predicted T stage, LNM, and pstage for EC patients. PET-CT-based radiomics is promising for improving the diagnosis and management of patients with EC.
Source: Insights into Imaging
Image Credit: iStock


