Humanizing radiology should be not a fashion but a way to rethink the profession of the radiologist instead. It represents not only a challenge but also an opportunity to redefine the role of the diagnostic radiologist as a physician primarily in the continuum of caring for patients.
From my point of view, there are great reasons to humanize healthcare and obviously radiology is one of the main specialities in need for this change.
Healthcare systems improvements in the last fifty years have been mainly technology-driven making radiology one of the medical specialities that has most benefited. Now it’s the time to boost our humanity at the same level as technology to balance our skills up.
High tech needs high touch
The invention of CT and MRI in the 20th century, both part of the most ground-breaking technological advances in medicine, changed not only the knowledge of many medical specialities but also the relationship between doctors and patients. Medical images are in the middle of more than 80% of medical decisions and this is why radiology is a central service in hospitals. Most patients go through the radiology service looking for a diagnosis.
On the other hand the radiologist’s job has become more complex during these years, with the number of images per exam being multiplied to exceed several thousands in some cases and at the same time having to master increasingly specialised knowledge.
However, complexity and technology improvements should run at the same speed as empathy. The clinical encounter between patient and the healthcare professional is the core activity of medical care. Empathy has been demonstrated to enhance the patient to doctor relationship, not only improving both the satisfaction of patient and doctor but also boosting diagnostic accuracy, since a huge part of the diagnosis relies upon the proper understanding of the clinical signs reported by the patient.
Transforming us into robots
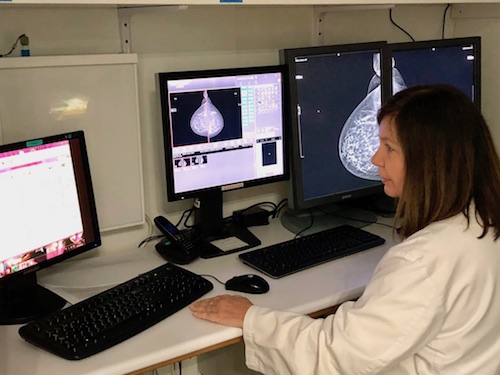
Electronic health records have granted us better access to the information of the patients and this is an advantage that at the same time carries the challenge of having to handle increasingly more information for each radiological report. Right now, the radiologist spends most of the time in dark reporting rooms interacting with a computer screen only. I imagine that many of them feel like robots although with a human weakness; every interruption in the process of reporting can potentially mean an error and that makes the radiologist a person who tends to reject human interaction in order to stay focused. Now radiologists are often “invisible” both to their patients and to their referring providers, and this is one of the main barriers in creating patient-centred care in radiology.
In recent radiology events such as the RSNA, ECR, and the SERAM conferences in Spain, artificial intelligence has been the trending topic and the most controversial discussion was whether artificial intelligence will or not replace radiologists. I'd bet that artificial intelligence will be a good assistant to the radiologist and an opportunity for getting closer to patient-centred radiology. We are physicians, and we must not forget it. Doctors should be doctors. Humanizing radiology begins by humanizing the profession. AI could leave the repetitive work to the machines achieving fewer errors than humans hence liberating the radiology professionals, so they can focus on humanizing medical care.
Humanizing radiology may also be an opportunity to avoid the burnout syndrome. The repetitive tasks such as reading images and writing reports can be one of the causes of burnout, while interacting with patients makes each case different and more interesting leading to higher satisfaction levels for the professional.
What will radiologists be doing then?
Radiologists using artificial intelligence will improve productivity and efficiency allowing more time for better communicating results to both the clinical teams and patients.
Both radiologists and radiographers must team up in dealing with images, diagnostics, data and also with patients. Let’s all of us explore communication skills in order to become experts in communication, technology and knowledge equally and as a result multiply the value of radiology.
Patients of the radiology service are usually scared; they are waiting for a sentence that might change their lives forever. Patients want to be valued, treated kindly, and shown compassion and empathy. Radiology services must consider patient’s emotional condition throughout the procedure providing better and clearer information in both the previous and later stages to the exam. The 21st-century patient is an empowered patient not compatible with the paternalist kind of medicine we have learned until now. Patient-centred care is not a wish—it is a must for them.
From a volume-based to a value-based practice
We have moved away from the origins of our profession switching the doctor-patient relationship for a doctor-patient´s images one. Patient-centred radiology is more efficient and better valued by patients. We must become more clinicians in order to gain the visibility we need to differentiate ourselves from the machines. AI is not the radiologist´s enemy—the enemy lives among us in the form of a report-centred radiologist. A movement is growing within radiology to adapt to the changing healthcare environment and focus on a patient-centred approach to improve patient satisfaction, quality, and safety.
In summary, humanizing radiology is the way to go back to doctor-patient relationships, to minimise the burnout syndrome cases and to make radiology a new exciting speciality, more clinical and adapted to the future era of artificial intelligence and empowered patients.


























