HealthManagement, Volume 1 - Issue 1, November-December 2007
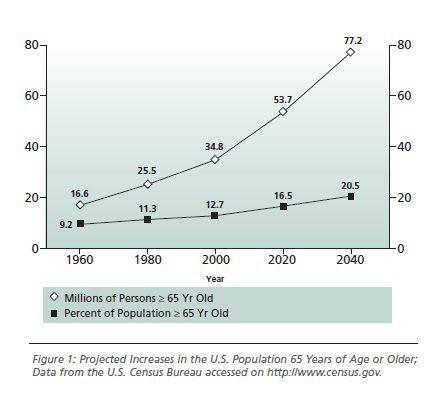
Multiple hospital admissions for acute decompensation are characteristic for congestive heart failure (CHF) patients, deleteriously affecting their quality of life and imposing a major burden on national healthcare costs. The direct costs of CHF-related hospitalisations amount to 2.7 billion Euro per year. Due to the demographic evolution of European societies, the number of hospitalisations is likely to further increase (see fig. 1).
Adherence to guidelines
will improve survival and reduce hospitalisation rates, thus lowering the
socio-economic burden. However, disease management strategies should not only
focus on drugs but comprise means to react to changes of health status and to
coordinate adaptation of the individual patient to both their disease and
environment. Telemedicine could be the key to integrate these prerequisites, to
facilitate communication with the patient and between caregivers to reduce
overall hospitalisation rates and costs. Furthermore, a recent meta-analysis
concluded that telemonitoring may be even more effective at shortening hospital
stays than reducing admissions, which would in turn have a considerable effect
on hospital capacity needed, patient turnover and patient costs to the
hospital.
The Concept of Telemedical Care
Predefined vital
parameters (e.g. weight, blood-pressure, heart-rate) are transmitted automatically
via modem to the telemedical centre, which can be contacted daily at any time
during the day. In case individual limits for vital parameters are exceeded an
alarm is triggered, allowing for immediate therapeutic action. Furthermore, to
enhance medical compliance and to detect changes in individual health status,
all patients could be proactively contacted alongside counselling on nutrition,
exercise and drug therapy in adjustment with the primary care physician.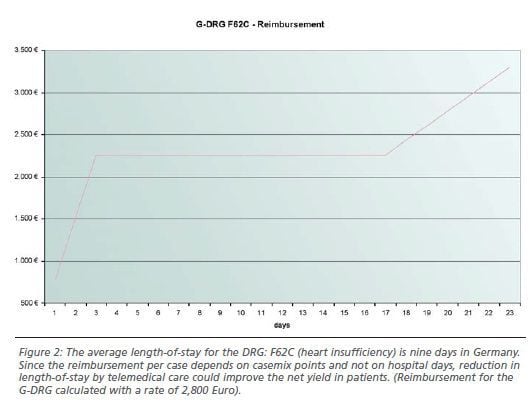
Clinical and Economical Effectiveness of Telemonitoring
Prospectively, 478
patients were included in the protocol, 270 (men: 85,5%; mean age 62,5 + 10
years; NYHA II, III, IV: 80 vs. 17 vs. 3%; main diagnosis: coronary heart
disease, hypertension, cardiomyopathy) of whom were monitored via telemedical
care and analysed in comparison to a matched control collective.
During an observation period of 3 months, hospitalisation (NYHA II, III, IV: 5,2 vs. 2,4; 8,1 vs. 3,0 und 2,4 vs. 1,2), length of stay (NYHA II, III, IV: 50,7 vs. 21,9; 78,4 vs. 27,5 und 23,0 vs. 10,9 days) and number of contacts to the GP (303,7 vs. 83,2) as well as to the cardiologist (105,3 vs. 30,4) were significantly reduced in the group of patients with telemedical care. Furthermore, increased compliance with a more appropriate adaptation of medication could be clearly demonstrated by standardised questionnaires.
Furthermore, an
independent economical analysis demonstrated a significant decrease of
CHF-related costs (about 3000 € per patient per year) in patients monitored via
telemedical care, predominantly due to a reduction of hospital days. The
according results can be seen in table 1.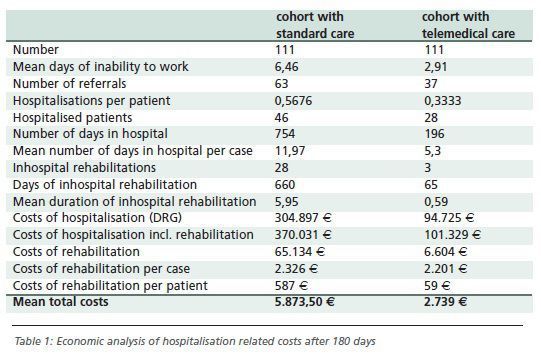
Impact of Telemedicine on Hospital Management
Since 2004, the German Diagnosis Related Groups system (G-DRG) has made compulsory, a prospective payment system for the purposes of budget determination and thus hospital financing in Germany. Based on the Australian Refined DRGs (AR-DRG), more than 1,000 different DRGs allow the categorisation of medical cases in homogeneous groups of equal economic expenditure. The sum of all case mix values per year corresponds to the budget of a hospital granted by the German health insurance companies. Therefore a clinic, specialised in heart failure treatment, might worry about losses by the decrease of the gained case mix points, as in-hospital days could be reduced by application of telemonitoring systems.
However, two aspects ensure that telemonitoring leads not only to improved patient care, but also to an improvement of the economic situation of a hospital. If a patient is hospitalised with the same DRG (due to repeated cardial decompensations) within a defined time interval to the same hospital, the hospital must connect both hospital stays to one case. Thus, the high costs of individual cases are no longer covered by the DRG reimbursement system. Therefore reduction of hospital readmission in patients monitored via telemedical care reduces the danger of non economical unification of individual heart failure cases.
The second aspect is the
clear decrease of length-of-stay (LOS) in hospitals due to telemedical care.
Since LOS is has little impact on the hospital’s reimbursement, a shortened
stay only leads to reduced costs for the individual case. Thus, the use of
telemonitoring by reduction of readmissions and LOS in heart failure patients
could improve the net yield in patients, as reimbursement per case depends on
case mix points and not on hospital days.
Implications
Following this analysis, telemedicine appears feasible both on economic and medical grounds. Intelligent algorithms for vital parameters allow efficient monitoring of multiple patients. More importantly, doctors can contact their patients earlier to prevent hospitalisations or to individually adjust medication. After a given hospitalisation and during titration of medication, a concept of technical de-escalation on a modular basis along with counselling measures appears highly likely to improve both patient awareness and CHF management. Finally, this implementation of telemedical care can work cost efficiently.





















