According to a new study (DEFUSE 3), thrombectomy for ischaemic stroke 6 to 16 hours after a patient was last known to be well plus standard medical therapy resulted in better 90-day functional outcomes than standard medical therapy alone among patients who had evidence of salvageable tissue on the basis of a formula that incorporated early infarct size and the volume of hypoperfused tissue on perfusion imaging.
DEFUSE 3 (Endovascular Therapy Following Imaging Evaluation for Ischaemic) was a randomised, open-label trial, with blinded outcome assessment, that compared endovascular thrombectomy plus standard medical therapy with standard medical therapy alone in patients with acute ischaemic stroke.
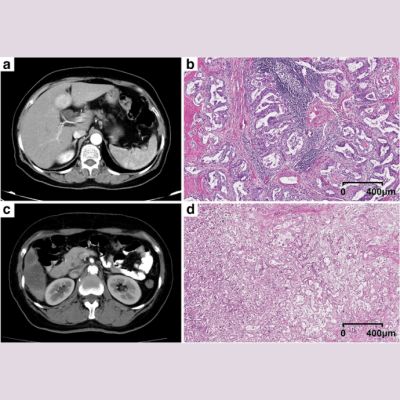
In the study, patients with proximal middle-cerebral-artery or internal-carotid-artery occlusion, an initial infarct size of less than 70 ml, and a ratio of the volume of ischaemic tissue on perfusion imaging to infarct volume of 1.8 or more were randomly assigned to endovascular therapy (thrombectomy) plus standard medical therapy (endovascular-therapy group) or standard medical therapy alone (medical-therapy group). The primary outcome was the ordinal score on the modified Rankin scale (range, 0 to 6, with higher scores indicating greater disability) at day 90.
The trial was conducted at 38 U.S. centres and terminated early for efficacy after 182 patients had undergone randomisation (92 to the endovascular-therapy group and 90 to the medical-therapy group). Endovascular therapy plus medical therapy, as compared with medical therapy alone, was associated with a favourable shift in the distribution of functional outcomes on the modified Rankin scale at 90 days (odds ratio, 2.77; P<0.001) and a higher percentage of patients who were functionally independent, defined as a score on the modified Rankin scale of 0 to 2 (45% vs. 17%, P<0.001).
Researchers found that the 90-day mortality rate was 14% in the endovascular-therapy group and 26% in the medical-therapy group (P=0.05). There was no significant between-group difference in the frequency of symptomatic intracranial haemorrhage (7% and 4%, respectively; P=0.75) or of serious adverse events (43% and 53%, respectively; P=0.18).
"The outcomes of thrombectomy in our trial were paradoxically better than those in many trials that treated patients within six hours after the onset of stroke. This finding may have been due to the selection of patients in the DEFUSE 3 trial with favourable collateral circulation and slower infarct growth," the researchers pointed out.
In this trial, the automated perfusion software (RAPID) was used to measure the volume of the early infarct and to measure hypoperfused volume. Recent studies suggest that infarct growth can occur over a period of several days in patients who do not have reperfusion of ischaemic regions.
In future trials, later time points could be considered to assess changes in infarct volume, the researchers said.
Source: The New England Journal of Medicine
Image Credit: Myohan
Latest Articles
ischaemic stroke, Thrombectomy, perfusion imaging
According to a new study (DEFUSE 3), thrombectomy for ischaemic stroke 6 to 16 hours after a patient was last known to be well plus standard medical therapy resulted in better 90-day functional outcomes than standard medical therapy alone among patients