HealthManagement, Volume 15 - Issue 2, 2015
The Role and Value of Incident Reporting in Radiology
Incident Reporting
Harm in Healthcare
A systematic review has shown that 9.2% of hospital inpatients experience harm from their care, with a median percentage of preventability of 43.5% (De Vries et al. 2008). Over half (56.3%) of patients experienced no or minor disability, whereas 7.4% of events were lethal. Operation- (39.6%) and medication-related (15.1%) events were most prevalent (De Vries et al. 2008). Many more patients are subject to near misses, with estimates ranging from 3 to 300 times as many near misses as adverse events (Barach and Small 2000; Runciman et al. 2007).
What is a Safety Incident?
A patient safety incident, (ie an ‘incident’), is defined as “an event or circumstance which could have resulted, or did result, in unnecessary harm to a patient” (Runciman et al. 2009). Incidents comprise both adverse events (in which a patient suffers physical or psychological harm, for example, a patient suffering stress from a misdiagnosis, or a reaction to intravenous contrast media) and ‘near misses’ in which the incident does not ‘reach’ the patient and no harm occurs. Near miss examples range from double-checking a patient’s identifier details on the request form with hospital records indicating a mix-up between two patients prior to imaging being conducted, or where a patient needs a right-sided nephrostomy, but is admitted and prepared for a left-sided nephrostomy with the error detected before commencement of the procedure and the correct side is treated. Near misses may not progress to adverse events, because they are intercepted by, and/or harm is mitigated by, systems containing many cross-checks and redundancies or vigilant people (eg discovering an incorrect procedure was planned during a surgical time out) or by chance and good luck (eg the radiologist did not read the referral with the incorrect side noted and performed the procedure on the correct side despite this not being what was requested) (Runciman et al. 2007). While comparison of near misses and adverse events may be confounded by hindsight bias, it is generally considered that the underlying systems failures for near misses are the same as for actual adverse events (World Alliance for Patient Safety 2005).
In the field of patient safety errors are defined as unintentional
consequences of either failure to carry out a planned action as intended, or
application of an incorrect plan (Runciman et al. 2009). Errors may occur by
doing the wrong thing (an error of commission) or by failing to do the right
thing (an error of omission) at either the planning or execution phase
(Runciman et al. 2009). James Reason has described the occurrence of errors in
a range of settings, including healthcare, aviation, mining and nuclear power
plants, by categorising errors as either latent (embedded within the system) or
active (occurring at the level of the operator) ( Reason 2000). These two
types of errors can reduce the effectiveness of the different layers of
defences designed to protect a system from loss. Most incidents are the result
of a sequence of events where each event in isolation would not cause harm.
Harm occurs when the flaws in the defences, usually both active and latent
errors, momentarily align in such a way that hazards are brought into damaging
contact with victims. Reason’s widely used Swiss cheese model (see Figure 1)
argues that focusing on active errors is flawed because systems weaknesses can
recur time and time again regardless of the operator (Reason 2000).
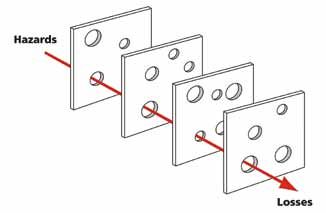
Figure 1. The Swiss Cheese Model
Source: Davidmack (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons.
The cheese slices represent the defences instituted to prevent errors and harm occurring. The holes in the cheese are the weaknesses of the defences that may allow harm to occur. Most incidents are prevented by one or more of the defences but occasionally all the defences fail and harm occurs (ie the holes in the cheese slices line up and the incident occurs)
Figure 2. WHO Conceptual Framework for the International Classification for Patient Safety
Why Reporting Incidents is Important
Incident reporting, when done well, can detect near misses and events where harm occurs (Anderson et al. 2013; World Alliance for Patient Safety 2005). Other safety tools and data sources may not capture near misses. The advantages of knowing about near misses include:
1. Near misses account for the majority of incidents;
2. They can act as an ‘early warning system’;
3. Information about how the incident was detected and mitigated before patient harm occurred can be obtained.
Incident data from near misses and adverse events can be useful in identifying risks that may allow harm to occur and in developing effective mitigation strategies to prevent similar events happening in the future.
Another benefit of incident reporting is its role in the development of a safety culture (World Alliance for Patient Safety 2005). The process of reporting is reflective, and this reflection on what happened, what could have happened and what stopped it being worse is important in creating a safety culture, ie one where actions are seen through a system ‘safety lens’ and staff are cognisant of safety in everything they do. Embedding vigilance about safety is an important distinguishing feature of high reliability organisations like nuclear aircraft carriers, nuclear power plants and air traffic control centres (Reason 2000). Such organisations are preoccupied with error and safety, and expect their staff to make errors, and therefore train their workforce to recognise errors and how to recover from them.
Characteristics of an Incident Reporting System
For an incident reporting system to be effective it needs to be easy and quick to use (World Alliance for Patient Safety 2005; Anderson et al. 2013). Reporting must be supported and encouraged by the organisation. In particular, reports are more likely to be submitted where the culture is just, ie non-punitive but accountable, key attributes of a safety culture (Reason 2000). Doctors are less likely to report when their identities are known, and this has been found to be due to fear of punishment; of being held responsible; or losing face to peers and seniors (Waring 2005). Making a reporting system anonymous and confidential encourages reporting. Having the incident reporting system managed by an organisation that is not a regulator or employer is reassuring to reporters and more likely to elicit information that will be helpful (Runciman 2002; Smith and Mahajan 2009).
A common language, or taxonomy, is helpful for classification, analysis and dissemination of findings. The World Health Organization’s International Classification for Patient Safety (ICPS) (World Alliance For Patient Safety Drafting group et al. 2009) (see Figure 2) provides a conceptual framework suitable for: comparing patient safety incident data across disciplines and between organisations on local, national and international levels; trending patient safety incident data; investigating patient safety incidents and identifying patient safety issues in different areas of care; examining the roles of system and human factors in patient safety; determining the applications and limitations of existing strategies to reduce risk to patients; identifying potential patient safety issues through evidence-based research; and developing priorities and preventative and corrective strategies.
Figure 3. Typical graphical presentation of data seen by the person who has reported an incident (i) time when incidents occur (ii) designation of reporter
Using an online reporting system saves costs in transcription and allows easier searching of data. Online forms can be adapted to elicit specific information depending on the data entered and ‘pick lists’ can simplify the process. Reporting is easier if there is ready access to the internet. Paper forms are still used by some agencies and have a role where internet access may not be available. Whatever system is used, data security is critical.
Open access to reporting enables anyone to report, not just radiologists. Nurses, radiographers and clerical staff all play an important role in patient safety, and their knowledge of incidents is invaluable in making patient care safer. Access for referring clinicians, patients and family members to report gives other insights into how healthcare can be improved. As patients rarely speak up during care (Weingart et al. 2005; Kinnunen and Sarantob 2013), having access to incident reporting may be the only way to capture data from a patient perspective.
Ideally collaboration between organisations and sharing of de-identified data will allow incidents to be entered once and distributed to the reporting system where the expertise is greatest.
Whilst much reporting is voluntary, some reports may be mandatory such as wrong patient, side or site procedures (Australian government Department of Health 2012), or where significant harm results from the incident. In a safety culture there is a great willingness to report incidents, even if seemingly trivial, as the benefit of reporting is widely understood and valued by management.
Reporting alone is not enough. A feedback or response system, ie classification of incidents to enable analysis and the development of alerts, warnings and solutions to prevent recurrence or mitigate the risk, is essential for an incident reporting system to be effective (Anderson et al. 2013). Timely feedback at the end of entering a report is also helpful in keeping those entering reports engaged.
Effective incident reporting results in safer care, better patient outcomes and cost savings as care is provided more efficiently and money is not spent on rectifying errors and treating harm.
Having a dedicated radiology incident reporting system supports the appropriate format, classification and analysis of patient safety data, and this allows the collection and understanding of information relevant to imaging. The outputs, such as alerts and warnings, will be relevant, practical and capable of being implemented and, therefore, more likely to be effective.
The Radiology Events Register (RaER)
The Radiology Events Register (www.raer.org.au) is the first national or internationaldedicated radiology incident reportingsystem. It was founded in 2006 by theRoyal Australian and New Zealand Collegeof Radiologists (RANZCR), and was fundedby the Federal government of Australiaas part of the R ANZCR’s Quality Use ofDiagnostic Imaging Program (QUDI) (Joneset al. 2010a). Currently RaER is funded bythe RANZCR, and the Australian PatientSafety Foundation (APSF) is contracted tomanage RaER. This provides independentmanagement and housing of the data (thusreassuring and protecting the reporters),and expertise in classifying incidents usinga validated patient safety classification.The data is subject to qualified privilege(statutory immunity) under relevant legislationin both Australia and New Zealand,meaning that it cannot be used in legalproceedings even if it could be identified.Although set up in Australia and NewZealand, there is no geographicalrestriction on reporting. RaER is not,however, a substitute for mandatoryreporting in hospitals and practices.
Figure 4. The imaging cycle showing the stages involved in imaging from formulating a clinical question that could be answered by medical imaging to the clinical action resulting from the radiologist’s report of the imaging.
To date we have over 4000 incidents from direct reports and data sharing with health departments, medical defence organisations and radiation regulators. The biggest hurdle for RaER is to encourage reporting. Doctors are not inclined to enter incidents into RaER or elsewhere and, as workloads are increasing, radiologists have little time to do anything other than report the radiology studies in front of them.
In order to encourage reporting, RANZCR has mandated incident reporting as part of the clinical radiology training programme and provides points for continuing professional development (CPD) for qualified radiologists. Incident reporting meets the requirement for reflective elements in CPD. Instant feedback is provided at the end of entering each case by means of a set of graphs showing a real-time summary of the types of incidents entered into RaER (see Figure 3).
Part of the data collection includes identifying where in the imaging cycle (see Figure 4) each incident is initiated and where it is detected (see Figure 5). This helps to identify the stages in the patient journey that are of higher risk (Jones et al. 2010b).
Figure 5. Phase of care where incidents were (i) initiated and (ii) detected
We have analysed reports to look for common causes and patterns that may be able to be mitigated. To date we have issued case reports with analysis of incidents and suggested risk mitigation strategies, and published papers in the peer-reviewed literature looking at errors in handover and communication. Papers on when and where errors occur and errors in neuroradiology have been presented at national and international conferences. The case reports published in RANZCR’s Inside News (www.ranzcr.edu.au/resources/newsletters/611current-edition)are popular and widely read. A full listof publications and presentations isavailable at www.raer.org.au/publications-presentations.html
Additionally, APSF convenes a multidisciplinary biennial conference, the Australasian Conference on Error in Medical Imaging, which promotes best practice and error reduction. These conferences are held in November, and include experts from radiology, patient safety and healthcare human factors.
Conclusion
Incident reporting is a key patient safety tool. RaER is at the international forefront of incident reporting in radiology, and the combination of radiologist expertise and the APSF’s skills in patient safety and human factors means that RaER outputs are a combination of best practice in patient safety and relevant and practical in radiology. The biggest challenge is increasing reporting rates. Experience in other industries shows that this is a matter of time, effective and continuous promotion and clearly demonstrating the benefits of reporting.For further information please go to www.raer.org.au
Key Points
- The Radiology Events Register (RaER) (www.raer.org.au) is the first radiology-specific incident reporting system to be established.
- Its purpose is to provide a platform to improve safety in radiology by recording, classifying and analysing incidents in a way that is relevant to radiology and that can result in education, alerts and other notices to raise awareness and help improve practice and safety in patient care.
- Incident reporting is a key safety tool in high-risk industries and is now widespread in healthcare. Many reporting systems are designed for health systems and do not cater for medical specialties such as radiology.
References:
Anderson JE, Kodate N, Walters R et al. (2013) Can incident reporting improve safety? Healthcare practitioners’ views of the effectiveness of incident reporting. Int J Qual Health Care, 25(2): 141–50.
Australian Government Department of Health (2012) Diagnostic imaging accreditation scheme practice accreditation standards. [Accessed: 17
April 2015] Available from http://www.health.gov.au/internet/main/publishing.nsf/Content/diagnosticimaging-accred-2-stand
Barach P , Small SD (2000) Reporting and preventing medical mishaps: lessons from nonmedical near miss reporting systems. BMJ, 320(7237): 759–63.
De Vries EN, Ramrattan MA, Smorenburg SM et al. (2008) The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care, 17(3): 216–23.
Jones DN, Benveniste KA, Schultz TJ et al. (2010a) Establishing national medical imaging incident reporting systems: issues and challenges. J Am Coll Radiol, 7(8): 582–92.
Jones DN, Thomas MJ, Mandel CJ et al. (2010b) Where failures occur in the imaging care cycle: lessons from the radiology events register. J Am Coll Radiol, 7(8): 593-602.
Kinnunen UM, Sarantob K (2013) It is time for selfincident- reporting for patients and their families in every health care organization: a literature review. Stud Health Technol Inform, 192: 92–6.
Reason J (2000) Human error: models and management. BMJ, 320(7237): 768–70.
Runciman W, Hibbert P, Thomson R et al. (2009) Towards an international classification for patient safety: key concepts and terms. Int J Qual Health Care, 21(1): 18–26.
Runciman WB (2002) Lessons from the Australian Patient Safety Foundation: setting up a national patient safety surveillance system--is this the right model? Qual Saf Health Care, 11(3): 246–51.
Runciman WB, Merry A, Walton M (2007) Safety and ethics in healthcare. Aldershot: Ashgate.
Smith AF, Mahajan RP (2009) National critical incident reporting: improving patient safety. Br J Anaest, 103(5): 623–5.
Waring JJ (2005) Beyond blame: cultural barriers to medical incident reporting. Soc Sci Med, 60(9): 1927–35.
Weingart SN, Pagovich O, Sands DZ et al. (2005) What can hospitalized patients tell us about adverse events? Learning from patient-reported incidents. J Gen Intern Med, 20(9): 830–6.
World Alliance For Patient Safety Drafting Group, Sherman H, Castro G et al. (2009) Towards an international classification for patient safety: the conceptual framework. Int J Qual Health Care, 21(1): 2–8.
World Alliance for Patient Safety (2005) WHO draft guidelines for adverse event reporting and learning systems: from information to action. Geneva: World Health Organization.

















