HealthManagement, Volume 3 - Issue 1, 2009
Telemedicine represents a good solution for the management of patients with cardiac problems. Telecardiology, in particular, guarantees continuity of care and the creation of integrated networks between acute hospitals and primary care, with a more rational and quicker management of patients. Additionally, telemedicine is particularly implemented where geographical barriers impinge on equity of access to health services. Italy, even if characterised by a high population density (approximately 200 inhabitants/km2), is rich in isolated and rural areas that suffer from a scarcity of healthcare resources.
Telecardiology in Italy
Telemedicine projects have existed across Italy since the 1990s. The most diffuse telemedicine services in Italy include telemonitoring of people with chronic conditions and teleconsultation for specific cardiac events. In particular, the main applications cover the following areas: telemonitoring of patients affected by chronic heart failure or hypertension, patients implanted with cardiac devices, teleconsultation for general practitioners and for emergency.
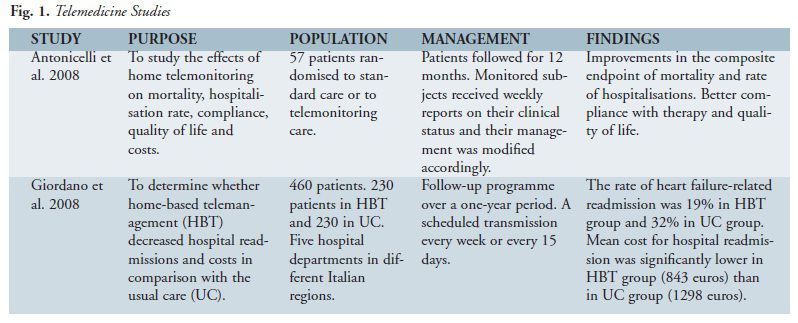
Chronic Heart Failure (CHF)
Usually after a cardiovascular related hospital discharge,
patients can be followed through a telemedicine programme. This management
model requires a portable device for ECG execution and subsequent transfer, by
an analogue or mobile telephone, to a call centre, which stores it and acts as
a point of contact between patients with hospital nurses and cardiologists. Hospital
staff is responsible for the clinical management of patients, providing consultations
or nursing triage, whereas the call centre provides technological and organisational
support and, if requested, offers clinical support 24 h/day, 365 days/year. All
patient data are stored on a web-server and available in order to keep the GP
informed and to support future investigations.
Hypertension
Self blood-pressure (BP) monitoring is acknowledged to play an essential role in the prevention and treatment of hypertension, with benefits both for clinical outcomes and for therapy optimisation (Parati et al. 2002). An inadequate BP control could be due to incorrect patient management. The usual model for the management of patients with hypertension through telemedicine systems requires a home BP monitoring device that allows a daily BP measurement and transmission over a mobile or analogue telephone line. Data are then reviewed by physicians, who can communicate the clinical conditions both to patients and to GPs and modify therapy during the ambulatory visits (e.g. every three months) based on the daily measurements of the previous period.
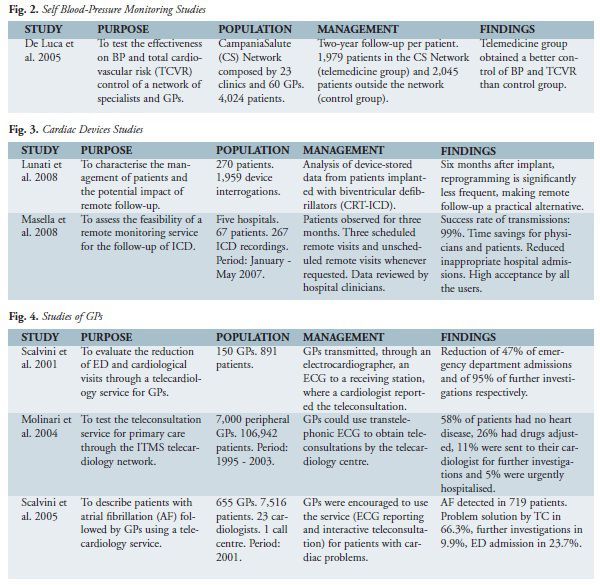
Cardiac Devices
The rise in new cardiac implantations leads to a consequent
increase in the number of follow-up visits in hospitals for patients implanted
with pacemakers (PM) or implantable cardioverter defibrillators (ICD). Remote monitoring of cardiac devices is an alternative to
intermittent visits. It allows early identification of device-related problems
and changes in rhythm and symptoms and reduces unnecessary visits. These
patients are well known by their specialists who, through the receipt of device
data remotely transmitted by patients at home, can quickly and appropriately decide
whether the patient needs a visit for device reprogramming, an emergency admission,
a change in therapy or nothing, with a consequent optimisation of healthcare
resources.
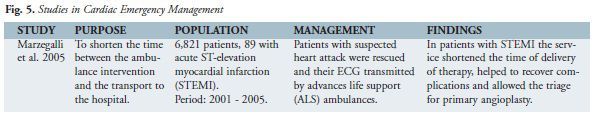
General Practitioners
Teleconsultation to support GPs is one of the most diffused applications. It allows provision of specialised support directly at the GP’s office with a lower use of hospital resources. Additionally, this service removes the obligation for patients to visit hospital, a benefit for patients who live in remote and isolated areas, or whose life conditions make the trip difficult. For example, the Telemaco project in the Lombardy region is currently testing a teleconsultation service for GPs localised in small mountain communities, which aims primarily at contrasting the depopulation of these isolated areas characterised by socioeconomic and infrastructural problems.
Traditionally, the management model involves GPs who, provided
with a portable electro cardiographer, ask the specialist for a teleconsultation
through a trans-telephone transmission of ECG recordings and a clinical request.
The network often involves a call centre with cardiologists available 24 h/day
offering ECG reporting and interactive teleconsultation with GPs.
Emergency
Cardiac emergency management through telemedicine is provided by
healthcare networks which involve ambulances, headquarters of 118 rescue
service and coronary care or cardiology hospital units. Transmission of the
patient's ECG and clinical parameters allows an early and accurate diagnosis
and the assessment of risk profile with a consistent reduction in time to
treatment and mortality rate.
Conclusions
Cardiology management models supported by telemedicine demonstrated benefits in terms of better follow-up, support for GPs’ daily activity, prevention of clinical changes, stimulation of self management of the illness, improvement of quality of life, reduction of rehospitalisation costs and quicker treatment in cardiac emergencies. In Italy telemedicine services are not routinely adopted and reimbursed by the national healthcare system. Telecardiology is still in the project stage and the scientific community is trying to provide the decision-maker with further evidence for its reimbursement.



















