A recent study by researchers at Penn Medicine shows that incisionless transcathether aortic valve replacement (TAVR) surgery can cut down the length of hospital stay by 30%. It was also shown that there was no impact on post-operative vascular complication rates when compared with conventional transfemoral TAVR, which requires an incision in the groin. The study is published in Circulation: Cardiovascular Interventions.
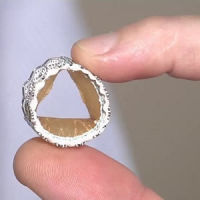
TAVR can be performed in two ways. One involves the insertion of a sheath into the femoral artery allowing the new valve to be threaded up to the patient's chest through a catheter. The second and more traditional approach inserts the same sheath but through an incision in the groin.
In recent years, physicians have been more inclined to use an approach that is incisionless and one which requires no more than a pin-prick to access the femoral artery. By using this approach, patients do not have any incisions and can leave the operating room without any trace of surgery. This study aimed to compare the two techniques in terms of vascular complications, outcomes and length of hospital stay.
The study was led by Jay Giri, MD, MPH, and assistant professor in the division of Cardiovascular Medicine at the Perelman School of Medicine at the University of Pennsylvania. The study involved 120 patients who had undergone TAVR via the traditional method and 211 patients who had percutaneous TAVR surgery. All patients were those treated at the Hospital of the University of Pennsylvania or Penn Presbyterian Medical Centre between 2007 and 2013.
It was observed that patients who received percutaneous surgery had a shorter post-procedural length of hospital stay as compared to those who underwent traditional TAVR surgery (7.5 versus 9.9 days). No differences in vascular complication such as haematomas, large bruises under the skin, dissections, tears in the vessel walls, and rupture of blood vessels rates were observed between the two procedures.
The researchers did however discover that vascular complications were related to the sex of the patient, and women seemed to be more at risk as compared to men. This aspect, however, requires further research. Vascular complications were also associated with larger valve introducer sheath outer diameter compared with the patient's artery diameter. This is because the introducer sheath can nick or disrupt the vessels in transit, resulting in complications for patients, regardless of the surgical approach used.
According to Giri, "While there are clinical circumstances when oversized sheaths must be used to accomplish a life-saving procedure, we discovered that, contrary to conventional wisdom, there really is no such thing as a safe oversize.”
This study is the first of its kind to evaluate the risk associated with increasing sheath oversizing. The study shows that vascular complication rates can decrease with improvement in technology and with a continuous decrease in sheath sizes in relation to artery diameter. The authors of the study give a word of caution when they say that careful pre-procedural planning with respect to sheath size and artery diameter is critical to decrease vascular complications.
Source: ScienceDaily
Image credit: American Heart Association
References:
Kadakia MB, Herrmann HC, Desai ND et al. (2014) Factors associated with vascular complications in patients undergoing balloon-expandable transfemoral transcather aortic valve replacement via open versus percutaneous approaches. Circulation: Cardiovascular Interventions, Published online before print July 15, 2014,
doi: 10.1161/CIRCINTERVENTIONS.113.001030
Latest Articles
TAVR
A recent study by researchers at Penn Medicine shows that incisionless transcathether aortic valve replacement (TAVR) surgery can cut down the length of ho...