Biobanks are made all the more valuable when the biological samples they hold can be linked to health information collected in research, electronic health records (EHR), or public health practice. Such data linkages, however, have raised concerns about patient privacy and data security. Incidentally, public trust in systems that share health information for research and healthcare practices is understudied.
In a recent study, Jodyn Platt and Sharon Kardia, both from the University of Michigan School of Public Health, examined characteristics of the general public that predict trust in health information sharing. They found that factors associated with increased trust include having experience with a primary care provider, having a favourable view of data sharing and believing that data sharing will improve the quality of healthcare, as well as psychosocial factors (e.g., altruism and generalised trust).
As expected, privacy concerns, but counterintuitively, knowledge about health information sharing are negatively associated with trust in health information systems. The results are published in the Journal of Personalized Medicine.
Methodology
To guide their investigation of the factors underlying the public’s trust in health information systems, the authors created a conceptual model (Figure 1) representing six areas anticipated to influence system trust. This model extends current research on trust in the health system by measuring trust at the individual and system levels, examining four key dimensions of trust:
The model evaluates the relationship between trust in the health system and: (1) knowledge of health information sharing; (2) experience with the health system; (3) attitudes and beliefs about privacy; (4) expectations of benefit; (5) psychosocial factors; and (6) demographic characteristics.
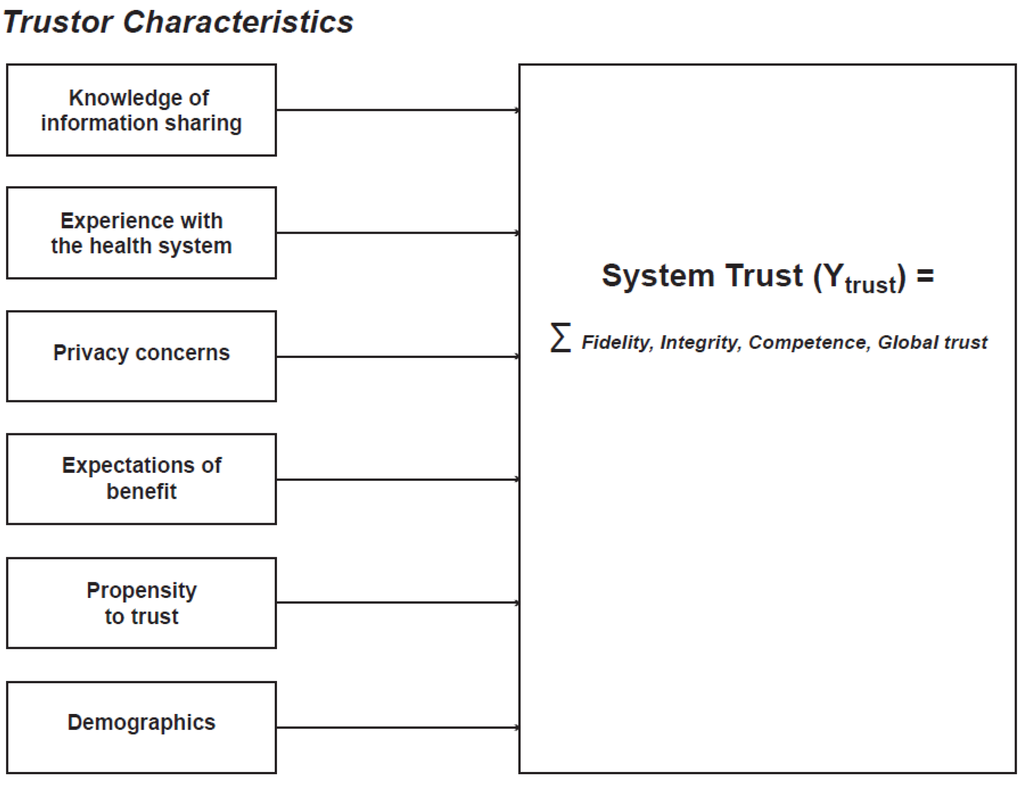
Figure 1. Conceptual Model
Knowledge of Health Information Sharing
In expanding the networks for health information, public engagement is identified as the key mechanism for building trust and acceptance, often under the assumption that this interactional form can overcome “knowledge deficits”. In short, “It is assumed that more or better knowledge or improved communication will enhance receptivity to innovations.” The authors assessed whether knowledge impacts trust in data sharing and if so, whether or not it increases support. They developed a set of fact-based questions to measure an individual’s knowledge about current, common policies and practices for data sharing among health care providers, insurers, researchers, and the public.
Experience with the Health System
Drawing on Luhmann’s theory that familiarity increases trust insofar as it reduces uncertainty, the authors assessed whether or not respondents had any contact with the health system either by seeing a primary health provider or having insurance.
Trustor Expectations
In the absence of direct knowledge about information use or experience with the health system, the public can still hold expectations for what the outcomes and benefits of the system will be. Private big data initiatives (e.g., Blue Health Intelligence) make the claim that expanding information infrastructure and making data sharing more efficient will improve the quality of healthcare and improve health. Understanding the public’s view of these goals and their general view of data sharing sheds light on the expectations they hold in entering into a relationship in which trust plays a central role.
Trustor Privacy Concerns
Survey research evaluating the public’s concerns about privacy suggests that it is a high salience issue, but that it is unclear to what extent fears about discrimination or a violation of privacy precludes participation in biobanks. There is some evidence that trust may increase if an individual is confident in the ability of a system to protect individual privacy.
Trustor Psychosocial Characteristics
Individual-level factors create world-views, embody social structures, and reflect the experience of everyday life. Based on these experiences, some individuals are more likely to exhibit trusting attitudes than others, regardless of the whether the context for trust is health-related or otherwise. Psychosocial factors such as self-esteem, optimism, self-efficacy, and a non-specific expectancy that people are reliable (i.e., general trust) are likely to reflect these generalised attitudes and beliefs.
Questionnaire Development
The authors created a 119-item survey of predictors and attributes of system trust, including the six trustor characteristics described above in the conceptual model as well as additional questions about trust in specific institutions (healthcare providers, researchers, and public health), quality of experience, perceived control, and adequacy of policy oversight.
To estimate and control for potential bias in participant responses due to the type of scale, the authors measured beliefs about privacy, psychosocial factors, and system trust using two scales. Half of the participants were asked questions on a four-point bipolar Agree/Disagree scale (Strongly Agree, Somewhat Agree, Somewhat Disagree, and Strongly Disagree). The other half responded to these questions using a four-point unipolar scale based on the prompt: “How true are the following statements?” The value labels that followed were: not at all true, somewhat true, fairly true, and very true. While there were some significant mean differences in the responses depending upon which scale was used, there was no difference in any of the regression relationships with System Trust.
In September 2013, the authors conducted an online Qualtrix survey of the general public (n = 447) using Amazon’s Mechanical Turk (MTurk) system.
Results and Conclusions
Having seen a primary care physician, having positive expectations of a benefit to health information sharing, and psychosocial factors (altruism, generalised trust) were found to have a positive association with trust. Having a primary care provider, but more importantly visiting that provider on one or more occasions within the year, predicts trust in the health system. This suggests that interpersonal relationships can have a positive effect on trust building in complex systems. As the health system becomes increasingly interconnected in the electronic space, it will be critical to find mechanisms and spaces in which trust can be negotiated and built person-to-person as it is in the doctor-patient relationship.
Having a generally favourable opinion about health information sharing had the greatest effect (β' = 1.36, p < 0.001). As a part of patient engagement or biobank recruitment, being able to demonstrate that health information sharing improves healthcare quality will be key in building public trust. Efforts should continue to identify the public’s expectations to understand how they might be met or betrayed in EHR and biobanking programmes.
Knowledge about data sharing practices, and having strong beliefs about the value of privacy were found to be negatively associated with trust. This finding provides an important caveat to community engagement research in the arena of biobanking and data sharing. Specifically, while engagement efforts have often revealed that a more informed public is more trusting and supportive of biobanking efforts, it is more likely the process of engagement that drives the support and not the top-down bestowing of information.
Future studies should examine system trust and its predictors using nationally representative samples. The current findings thus far suggest that decision-makers in health information sharing need to explore mechanisms and policy options — such as community consultation approaches or education via partnership models — that effectively build or sustain trust as they develop partnerships to work across systems.
Image Credit: Edubloggers.org
In a recent study, Jodyn Platt and Sharon Kardia, both from the University of Michigan School of Public Health, examined characteristics of the general public that predict trust in health information sharing. They found that factors associated with increased trust include having experience with a primary care provider, having a favourable view of data sharing and believing that data sharing will improve the quality of healthcare, as well as psychosocial factors (e.g., altruism and generalised trust).
As expected, privacy concerns, but counterintuitively, knowledge about health information sharing are negatively associated with trust in health information systems. The results are published in the Journal of Personalized Medicine.
Methodology
To guide their investigation of the factors underlying the public’s trust in health information systems, the authors created a conceptual model (Figure 1) representing six areas anticipated to influence system trust. This model extends current research on trust in the health system by measuring trust at the individual and system levels, examining four key dimensions of trust:
- Fidelity - captures attitudes about the benevolence of the health system, i.e., the ability of the system to prioritise the needs and interests of the public;
- Integrity - defined as honesty, captures confidence in upholding the principles of non-deception;
- Competency - refers to the ability and expertise to minimise errors and achieve goals; and
- Global trust - an integrative concept that captures an individual’s general perception of trustworthiness.
The model evaluates the relationship between trust in the health system and: (1) knowledge of health information sharing; (2) experience with the health system; (3) attitudes and beliefs about privacy; (4) expectations of benefit; (5) psychosocial factors; and (6) demographic characteristics.
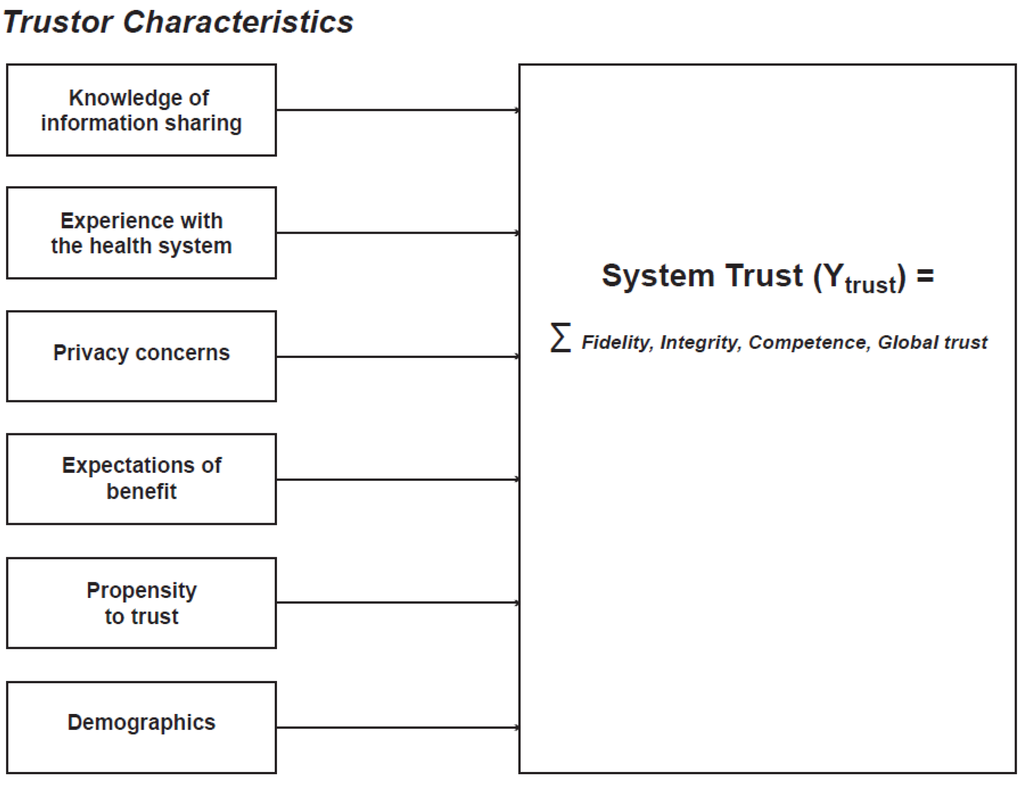
Figure 1. Conceptual Model
Knowledge of Health Information Sharing
In expanding the networks for health information, public engagement is identified as the key mechanism for building trust and acceptance, often under the assumption that this interactional form can overcome “knowledge deficits”. In short, “It is assumed that more or better knowledge or improved communication will enhance receptivity to innovations.” The authors assessed whether knowledge impacts trust in data sharing and if so, whether or not it increases support. They developed a set of fact-based questions to measure an individual’s knowledge about current, common policies and practices for data sharing among health care providers, insurers, researchers, and the public.
Experience with the Health System
Drawing on Luhmann’s theory that familiarity increases trust insofar as it reduces uncertainty, the authors assessed whether or not respondents had any contact with the health system either by seeing a primary health provider or having insurance.
Trustor Expectations
In the absence of direct knowledge about information use or experience with the health system, the public can still hold expectations for what the outcomes and benefits of the system will be. Private big data initiatives (e.g., Blue Health Intelligence) make the claim that expanding information infrastructure and making data sharing more efficient will improve the quality of healthcare and improve health. Understanding the public’s view of these goals and their general view of data sharing sheds light on the expectations they hold in entering into a relationship in which trust plays a central role.
Trustor Privacy Concerns
Survey research evaluating the public’s concerns about privacy suggests that it is a high salience issue, but that it is unclear to what extent fears about discrimination or a violation of privacy precludes participation in biobanks. There is some evidence that trust may increase if an individual is confident in the ability of a system to protect individual privacy.
Trustor Psychosocial Characteristics
Individual-level factors create world-views, embody social structures, and reflect the experience of everyday life. Based on these experiences, some individuals are more likely to exhibit trusting attitudes than others, regardless of the whether the context for trust is health-related or otherwise. Psychosocial factors such as self-esteem, optimism, self-efficacy, and a non-specific expectancy that people are reliable (i.e., general trust) are likely to reflect these generalised attitudes and beliefs.
Questionnaire Development
The authors created a 119-item survey of predictors and attributes of system trust, including the six trustor characteristics described above in the conceptual model as well as additional questions about trust in specific institutions (healthcare providers, researchers, and public health), quality of experience, perceived control, and adequacy of policy oversight.
To estimate and control for potential bias in participant responses due to the type of scale, the authors measured beliefs about privacy, psychosocial factors, and system trust using two scales. Half of the participants were asked questions on a four-point bipolar Agree/Disagree scale (Strongly Agree, Somewhat Agree, Somewhat Disagree, and Strongly Disagree). The other half responded to these questions using a four-point unipolar scale based on the prompt: “How true are the following statements?” The value labels that followed were: not at all true, somewhat true, fairly true, and very true. While there were some significant mean differences in the responses depending upon which scale was used, there was no difference in any of the regression relationships with System Trust.
In September 2013, the authors conducted an online Qualtrix survey of the general public (n = 447) using Amazon’s Mechanical Turk (MTurk) system.
Results and Conclusions
Having seen a primary care physician, having positive expectations of a benefit to health information sharing, and psychosocial factors (altruism, generalised trust) were found to have a positive association with trust. Having a primary care provider, but more importantly visiting that provider on one or more occasions within the year, predicts trust in the health system. This suggests that interpersonal relationships can have a positive effect on trust building in complex systems. As the health system becomes increasingly interconnected in the electronic space, it will be critical to find mechanisms and spaces in which trust can be negotiated and built person-to-person as it is in the doctor-patient relationship.
Having a generally favourable opinion about health information sharing had the greatest effect (β' = 1.36, p < 0.001). As a part of patient engagement or biobank recruitment, being able to demonstrate that health information sharing improves healthcare quality will be key in building public trust. Efforts should continue to identify the public’s expectations to understand how they might be met or betrayed in EHR and biobanking programmes.
Knowledge about data sharing practices, and having strong beliefs about the value of privacy were found to be negatively associated with trust. This finding provides an important caveat to community engagement research in the arena of biobanking and data sharing. Specifically, while engagement efforts have often revealed that a more informed public is more trusting and supportive of biobanking efforts, it is more likely the process of engagement that drives the support and not the top-down bestowing of information.
Future studies should examine system trust and its predictors using nationally representative samples. The current findings thus far suggest that decision-makers in health information sharing need to explore mechanisms and policy options — such as community consultation approaches or education via partnership models — that effectively build or sustain trust as they develop partnerships to work across systems.
Image Credit: Edubloggers.org
References:
Platt J, Kardia S (2015) Public Trust in Health Information Sharing: Implications for Biobanking and Electronic Health Record Systems. J.
Pers. Med. 2015, 5(1), 3-21; doi:10.3390/jpm5010003
Latest Articles
EHR, electronic health records, biobanks, data sharing, trust
Biobanks are made all the more valuable when the biological samples they hold can be linked to health information collected in research, electronic health...



























