Researchers at the University of Texas in Dallas (UTD) have found that breast cancer diagnoses can be improved when radiologists consider a patient’s statistically-weighted risk profile while examining her mammogramme. The new approach should result in a reduction of missed diagnoses and false positives. The study was presented this week at the Advances in Decision Analysis conference, sponsored by the Institutes for Operations Research and the Management Sciences (INFORMS), at Georgetown University in Washington, DC.
The Role of Risk in Readings
There are several risk factors for breast cancer which enter into a patient’s risk profile. Age, ethnicity, family history and reproductive history all influence a woman’s chances of developing the disease. For radiologists evaluating a woman’s mammogramme for signs of breast cancer, it can be helpful to be aware of the risk profile to minimise both false negatives and false positives. The use of logical decision-making methods, such as those investigated by the INFORMS Decision Analysis Society, has the potential to improve outcomes for patients.
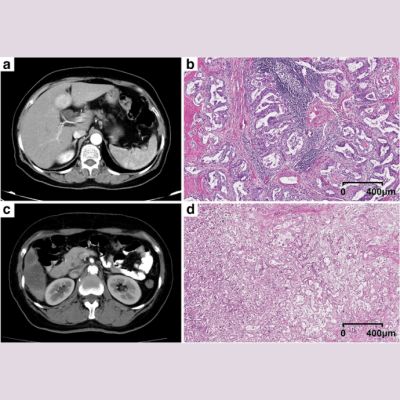
The UTD researchers accessed a clinical dataset provided by the Breast Cancer Surveillance Consortium. Three groups of mammogramme readings were analysed, based on their decision performance: mammogramme-only readings, without risk profile information; mammogramme readings followed by consultation of the patient’s risk profile (‘unbiased readings’); and readings which involved consultation of the risk profile during the mammogramme evaluation (‘biased readings’). There was a subsequent examination of the conditions in which biopsy decisions could be improved by risk profile data.
Bias: Harmful or Helpful?
Clinical evidence has been inconclusive about the inclusion of risk profile information during mammogramme analysis. While it is potentially helpful to the radiologist, some believe that readings are ‘biased’ by the profile data. Bias can be helpful in improving accuracy and lowering the number of false negatives, but it can also cause harm if it raises the number of false positives. Considering the prevalence of breast cancer as the second most deadly non-skin cancer, accuracy is vital. There were 232,000 diagnoses and approximately 39,000 deaths from breast cancer in 2013.
Using a numerical analysis technique called linear opinion pooling, a decision science method, the researchers assigned weights to aggregate probability estimates. In the end, they found that the radiologists’ use of risk profile information, along with the statistical weighting, reduced false negatives by 3.7 percent and false positives by 3.23 percent. Thus, more women were alerted to early-stage cancer which might have otherwise gone undiagnosed, and patients who did not have cancer were spared the stress of false diagnoses. Unnecessary healthcare expenses were also reduced.
INFORMS is an international leader in analytics and operations research, developing and promoting best practices through professional development and collaboration. Its Decision Analysis Society was formed in 1980; current membership is approximately 1,000 professionals. This year's Advances in Decision Analysis conference took place between 16 and 18 June.
Latest Articles
Imaging, Mammography, breast cancer screening, risk factor, breast imaging, mammogramme
Researchers at the University of Texas in Dallas (UTD) have found that breast cancer diagnoses can be improved when radiologists consider a patient’s sta...