Patient experience is becoming increasingly prioritised in line with the focus on value-based care. Given the scope of imaging services, diagnostic radiologists are better positioned to seize opportunities to innovate in patient experience than is readily apparent, says a review article in the journal Current Problems in Diagnostic Radiology.
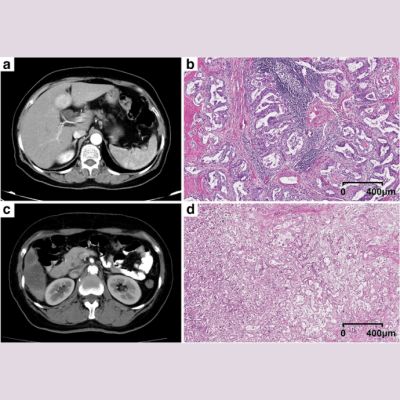
Radiology departments touch nearly every patient engaging with the healthcare system spanning the inpatient, outpatient, and emergency care settings, providing an enormous potential scale of impact for improvements in patient experience. The series of steps spanning a patient’s initial symptom or condition requiring imaging to the communication of an actionable imaging result has been collectively termed the “imaging value chain.”
The article says identifying which components of the imaging value chain represent the most potent modifiers of patient experience could facilitate targeted improvement efforts. Regarding exam scheduling, for example, radiology departments can attempt to allow flexibility in appointment timing and adopt mobile and online interfaces to streamline the scheduling process.
"During the examination, radiologic technologists are vital in educating patients regarding what to expect, in addition to ensuring patients’ physical and emotional comfort during positioning and image acquisition," the article explains. "Following the examination, a brief discussion of preliminary findings by the radiologist, when practical, also represents an opportunity to assuage patient anxiety while implicitly conveying that their images have entered the hands of a caring physician."
In addition, the field of radiology has traditionally been an innovator in health information technology (IT). Since incorporation of health IT tools into patient care is becoming increasingly prioritised in healthcare legislation, this signals an opportunity for radiologists to continue capitalising on their collective technological vision. In this regard, radiologist’s input toward the imaging components of electronic patient portals could aim to enhance patient understanding of imaging results. This could be achieved, for example, through embedded educational tools that clarify complex terminology and imaging findings.
In addition to facilitating image interpretation, the article says, artificial intelligence tools could be leveraged to noninterpretive ends such as workflow optimisation and improved patient access to care.
"Carefully vetted opportunities for direct patient engagement would likely expand the reach of diagnostic radiologists as members of integrated health systems," according to the article. Innovative patient engagement mechanisms such as the creation of a diagnostic radiology consultation clinic have thus far been well received by patients and referring providers in pilot studies. Models such as the consultation clinic or virtual patient encounters could ease the burden on referring physicians and appropriately delegate to radiologists the task of explaining technically complex results or incidental findings.
"Whether through process improvements in the logistics of obtaining an imaging study, creation of novel digital tools to streamline care, or direct engagement with patients to allay their fears, ample opportunities exist to optimise the patient experience in radiology," the article concludes.
References:
Gottumukkala RV, Le TQ, Duszak Jr R, Prabhakar AM (2018) Radiologists Are Actually Well Positioned to Innovate in Patient Experience. Curr Probl Diagn Radiol 47(4):206–208. https://doi.org/10.1067/j.cpradiol.2017.09.010
Latest Articles
Radiologists, patient experience, value-based care
Patient experience is becoming increasingly prioritised in line with the focus on value-based care. Given the scope of imaging services, diagnostic radiologists are better positioned to seize opportunities to innovate in patient experience than is readily