ICU Management & Practice, ICU Volume 15 - Issue 3 - 2015
To monitor nutrition is not
complicated or difficult. What is more problematic is to monitor nutritional
risk and to define the purpose or target for nutrition, especially in the
critically ill patient. The present analysis is designed to be useful for
nutritional support for critically ill patients admitted to the ICU. The heterogeneity
of the patient population is the initial and main problem for nutrition
support. However, if nutrition support is individualised, monitoring will be
rather straightforward. So the initial step will be to identify the critically ill
patients who are at nutritional risk and in whom nutrition makes a difference.
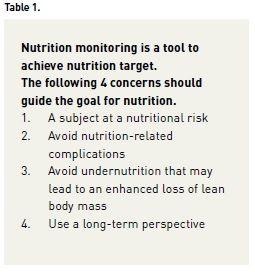
The purpose of nutrition is of course to improve patient outcome. Four general guidelines may be proposed (see Table 1):
(i) to identify subjects at nutritional risk,
(ii) to avoid nutrition-related complications,
(iii) to avoid undernutrition that may lead to an enhanced loss of lean body mass, and
(iv) to have a longterm perspective.
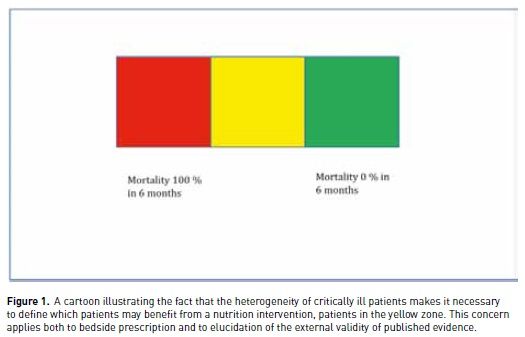
Heterogeneity
The heterogeneity of critically ill patients is perhaps best illustrated by the simplistic cartoon in Figure 1. We propose that there are three groups of critically ill patients in relation to nutrition and outcome;
1. those that have a favourable outcome regardless of nutrition,
2. those that have an unfavourable outcome regardless of nutrition and
3. those that may benefit from nutrition, if given correctly.
The groups of patients that are going to have a favourable or unfavourable outcome, regardless of nutrition support, are perhaps not always possible to identify bedside on the day of ICU admission. Conceptually, however, it is important to think in these terms when evidence is evaluated in conjunction with trials investigating nutrition support and outcome. At least retrospectively it is usually possible to identify wellnourished subjects with a very low risk for an unfavourable outcome, as well as subjects with a very low chance of a favourable outcome. If these groups of patients constitute a large proportion of a cohort studied, the chance or possibility to detect a nutrition-related effect on outcome is of course low. It may even result that poor nutrition monitoring and non-individualised nutrition in the high-risk patient cohort induce nutritional risks that totally outweigh the possible benefits.
Another dimension of heterogeneity is the uneven distribution of length of ICU stay. A majority of critically ill patients are short-stayers, while a minority of long-stayers are consuming the vast majority of ICU days. Here differences in case mix and healthcare systems must be considered when the external validity of nutrition studies are discussed. Heterogeneity also comes with the time in the ICU and the variable duration of illness before admission.
Nutritional Risk
The idea of starting with the discussion over heterogeneity is to encourage triage to identify the patients who are at nutritional risk and in whom nutrition matters. It is perhaps not always possible at admission, but within a time period of 4-7 days, they should be identified and subjected to individualised nutrition care including monitoring. Before this time the routines of the unit should focus on “low-risk - maximum benefit interventions”.
The evidence that under nutrition may be harmful in critical illness is purely observational. Although malnutrition is associated with unfavourable outcomes in health as well as disease, the predictive value in critical illness is difficult to separate from a number of comorbidities strongly associated with complications and unfavourable outcomes (Moreno et al. 2005).
In particular, nutritional treatment of malnutrition in critical illness is perhaps supported by “common sense”, but to a lesser degree by evidence. Nevertheless to try to minimize further aggravation of malnutrition for malnourished long-stayers in the ICU is a strategy embraced by most opinion leaders. However, this is a challenging task as this group of subjects is probably also the one most prone to nutrition-related complication. Hence perhaps the group to benefit the most from nutrition monitoring – the present topic.
To identify patients at nutrition risk may be a bedside challenge. Definitions developed for non-critically ill subjects may be of limited help (Kondrup et al. 2003). The Nutrition Risk in Critically Ill (NUTRIC) score, recently developed for the critically ill, does not separate the risk from malnutrition from the risk from co-morbidities (Heyland et al. 2011). Nevertheless, the NUTRIC score may presently be the best tool to use. It must also be considered that risk related to nutrition status may change over time. A selection of patients considered to be at nutrition risk may be the best use of resources, but this has never been properly demonstrated. Perhaps this level of care should be offered to everybody, but the workload involved should not be underestimated. A close daily evaluation combined with intense monitoring and reconsideration of treatment will consume hours of nurses’, dieticians’ and doctors’ time. Therefore a selection of patients is most probably necessary.
Nutrition-Related Complications
Among nutrition-related complications, overnutrition is probably the most common. This is well known and documented already in the Veterans study, and also from a number of observational reports (Veterans Affairs Total Parenteral Nutrition Cooperative Study Group 1991). The problem when discussing overnutrition is the difficulty in defining it. Most will agree that feeding calories above the energy expenditure is to be considered as overfeeding. This definition, however, contains two problems: 1) energy expenditure is often not known, and 2) it is not self-evident that overfeeding is avoided also when feeding is in accord with energy expenditure. Literature on this topic is not conclusive as cohorts of patients reported are a mixture of short-stayers and long-stayers, with a variable level of nutrition status and finally including subjects in the acute phase as well as a more stabilised phase.
It is very difficult to state that overnutrition is avoided without actually measuring energy expenditure, unless an obvious hypocaloric feeding is practised. Hypocaloric feeding may be practised in non-malnourished subjects for a limited period of time (Krishnan et al. 2003). A recent study demonstrated no benefit and no harm from such a protocol, but there is no validity outside the group of relatively young and well-nourished patients actually studied (Arabi et al. 2015).
Individualised Protocol
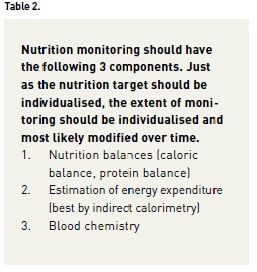
The basis for individualised nutrition is to have an adequate recording of intake and thereby the possibility to calculate a caloric balance and a protein balance in parallel to the fluid balance practised in most ICUs (Preiser et al. 2015). It is particularly important to also consider nonnutrition calories (the caloric content of solution for antibiotics, sedatives etc.). Still balance calculations can be problematic when considering volume and caloric content of vomit, diarrhoea, and drainages. There may also be concerns over the nutrition value of blood products. Overall it is recommended to not make these balances more complicated than necessary; still when extraordinary intakes or losses are at hand the calculated balance may from time to time be kept in mind. The value of regular measurement of urinary nitrogen losses is debatable, but when a high protein intake on a level above the general recommendations of 1.2-1.5 g/kg/day is practised, the indication also to follow urinary urea excretion as a safety parameter increases. Again, the main difficulty with individualising nutrition and calculation of a correct balance is the determination of the individual’s nutritional need.
Caloric Needs
Estimation of the caloric need remains the key question when dealing with a subject at nutrition risk. The use of indirect calorimetry is controversial, but must be considered to be gold standard. The criticism is that reproducibility of measurements is not good enough and that the technique is not open to all patients (those not on mechanical ventilation, with a high oxygen fraction, with airway leakages etc.). But at the end of the day there is probably no better option. In particular for subjects with extremes in BMI it is very difficult to estimate energy expenditure by formulas or by guessing. It is advised to use indirect calorimetry not only in very restricted cases, because there is a learning curve in instrument handling and if used very rarely readings may be less reliable. Repeated readings in subjects at nutrition risk add value when a trend becomes available. Still with the estimated energy expenditure in hand the question remains how to translate this into a calorie number.
Protein Needs
Recently a number of authors have advocated a high protein (amino acid) intake in critical illness (Hoffer and Bistrian 2012). Again there is no evidence outside observational and retrospective reports, and the same “chicken and egg” matter as for the relevance of an energy deficit exists. Even the guidelines from nutrition societies of 1.2-1.5 g protein per kg and 24h deviate from the recommendations for healthy individuals and are supported by very little evidence (Kreymann et al. 2006, Singer et al. 2009). To recommend an intake above that level without a proper study protocol and nutrition monitoring is not compatible with patient safety.
Long-Term Perspective
The long-term perspective means that after ICU discharge nutritional support must also be considered. It is of course quite meaningless to institute an ambitious nutrition regimen in the ICU, just to abandon it after discharge. Many studies are rightly criticised for evaluating a nutrition intervention during ICU stay in terms of long term (3-12 months) outcomes, without any information of nutrition intake during the post-ICU period (Griffiths et al. 1997; van Zanten et al. 2014). The assumption that non-recorded nutrition is comparable between groups outside the protocolised period is not very convincing. So if a decision is made to individualise nutrition for critically ill subjects at nutritional risk during ICU stay, a post-ICU follow-up plan is also needed. In institutions with a nutrition team, this may come automatically but otherwise a plan for nutrition should cover the entire period when the subject is considered to be at nutrition risk, both within the hospital, but also in the post-hospital rehabilitation period.
Blood Chemistry
The third cornerstone of nutrition monitoring is to use blood analyses to reflect the metabolism of macro-nutrients. The basis will be blood glucose, plasma triglycerides, plasma urea and plasma ammonia. Frequency of sampling will be related to how the results of these blood tests will be interpreted, to guide prescriptions and/or as safety parameters.
Blood glucose is best available on the blood gas analyses, usually monitored for respiratory purposes (Wernerman et al. 2014). If tight glucose control is practised, hourly measurements are usually necessary, at least in the initial phase. A better understanding of the need of exogenous glucose and the mechanism behind insulin resistance may suggest a more differentiated approach to glucose control related to intake (Soeters and Soeters 2012).
Triglycerides, urea and ammonia are more commonly used as safety monitoring. With very high intakes of protein (amino acids), plasma urea (and also urinary urea) may be used to guide protein dosing. Frequency of sampling in an ICU setting may be each 2nd to 5th day, unless there is kidney or liver failure, which may motivate daily measurements. Elevated plasma triglycerids may motivate restriction of fat intake. This is more common with parenteral fat intake, and the mechanism is not fully understood. Consequently the cut-off level when to reduce fat intake is controversial. For subjects with extensive external fluid (and tissue) losses, with metabolic conditions, and for extreme long-stayers, a more differentiated testing may be motivated, covering vitamins,trace elements and individual amino acids. Such monitoring should always be individualised, in the extent of testing as well as in frequency of testing (Gagnon et al. 2015).
Conclusion
It is not meaningful to discuss nutrition monitoring unless a target or goal for nutrition treatment is established. To define the goal, the first step should be to decide whether or not the individual patient is at nutritional risk or not. The nutrition should thereafter be individualised, should avoid nutrition-related complications, and should be part of a long-term perspective. Nutrition balance, estimation of energy expenditure, and blood chemistry checks should then be applied according to the goal defined.
References:
Arabi YM, Aldawood AS, Haddad SH et al. (2015) Permissive underfeeding or standard enteral feeding in critically ill adults. N Engl J Med, 372(25): 2398-408.
Gagnon G, Voirol P, Soguel L et al. (2015) Trace element monitoring in the ICU: quality and economic impact of a change in sampling practice. Clin Nutr,34(3): 422-7.
Griffiths RD, Jones C, Palmer TE (1997) Six-month outcome of critically ill patients given glutamine-supplemented parenteral nutrition. Nutrition, 13(4): 295-302.
Heyland DK, Dhaliwal R, Jiang X et al. (2011) Identifying critically ill patients who benefit the most from nutrition therapy: the development and initial validation of a novel risk assessment tool. Crit Care, 15(6): R268.
Hoffer LJ, Bistrian BR (2012) Appropriate protein provision in critical illness: a systematic and narrative review. Am J Clin Nutr, 96(3): 591-600.
Kondrup J, Allison SP, Elia M et al. (2003) ESPEN guidelines for nutrition screeningb2002. Clin Nutr, 22(4): 415-21.
Kreymann KG, Berger MM, Deutz NE et al.(2006) ESPEN Guidelines on Enteral Nutrition:Intensive care. Clin Nutr, 25(2): 210-23.
Krishnan JA, Parce PB, Martinez A et al. (2003) Caloric intake in medical ICU patients: consistency of care with guidelines and relationship to clinical outcomes. Chest, 124(1): 297-305.
Moreno RP, Metnitz PG, Almeida E et al. (2005) SAPS 3—From evaluation of the patient to evaluation of the intensive care unit. Part 2: Development of a prognostic model for hospital mortality at ICU admission.Intensive Care Med, 31(10): 1345-55.
Preiser JC, van Zanten AR, Berger MM et al. (2015) Metabolic and nutritional support of critically ill patients: consensus and controversies. Crit Care, 19: 35.
Singer P, Berger MM, Van den Berghe G et al. (2009) ESPEN Guidelines on Parenteral Nutrition: intensive care. Clin Nutr, 28(4): 387-400.
Soeters MR, Soeters PB (2012) The evolutionary benefit of insulin resistance. Clin Nutr, 31(6): 1002-7.
van Zanten AR, Sztark F, Kaisers UX et al. (2014) High-protein enteral nutrition enriched with immune-modulating nutrients vs standard high-protein enteral nutrition and nosocomial infections in the ICU: a randomized clinical trial. JAMA, 312(5): 514-24.
Veterans Affairs Total Parenteral Nutrition Cooperative Study Group (1991) Perioperative total parenteral nutrition in surgical patients. N Engl J Med, 325(8): 525-32.
Wernerman J, Desaive T, Finfer S et al. (2014) Continuous glucose control in the ICU: report of a 2013 round table meeting. Crit Care, 18(3): 226.




















