ICU Management & Practice, ICU Volume 14 - Issue 2 - Summer 2014
Author

Pravin Amin,MD, FCCM
Head, Department of Critical Care Medicine
Bombay Hospital Institute of Medical Sciences
Mumbai, India
Globally neurocritical care is a well-established field in medicine. In India this discipline has developed in the major cities. However, elsewhere it is found wanting. The high incidence of head trauma and stroke and advances in neurosurgical techniques clearly warrant the need for neurocritical care units. The morbidity and mortality associated with head trauma and stroke will certainly reduce if state-of-the art neurocritical care centres are established across the country.
Introduction
India is a vast country with a population of over 1.2 billion people, still rising by about 18 million a year. Healthcare provision is not a centralised process. The government plays a very small role in healthcare delivery, nor does it have control over the non-governmental sector. Only a small proportion of publicly-funded government hospitals are able to provide state-of-the-art care, whereas a large percentage of public hospitals only provide basic care. This is due to the fact that India currently spends only 3.9 per cent of its GDP on publicly-funded healthcare. Most healthcare in India is currently provided via the private sector. Because of a lack of affordable insurance protection it is principally funded via out-of-pocket payments.
Understandably, private institutions provide most critical care services in this part of the world. There are large numbers of neurocritical centres across the country, but most neurocritical care patients are treated in general ICUs. In an Internet-based survey conducted by the author in 2013 with a web-based Indian Critical Care discussion group, of the 162 respondents 59 (36.42%) stated they had exclusive neurocritical care units (Amin 2014).
Critical care in India started in the early 1960s, and was introduced in the city of Mumbai. It slowly and gradually spread to other cities and towns. A formal society of critical care, the Indian Society of Critical Care Medicine (ISCCM) was formed in 1993, and now has around 7000 members.
The Neurological Society of India (NSI) was founded by eminent neurosurgeons and neurologists in 1951. The NSI currently has 2,565 members, of whom 1,983 are neurosurgeons and the rest are neurologists. In 1992 the neurologists decided that they certainly had to have an identity of their own, which led to the formation of the Indian Academy of Neurology, which now has a membership of 1,323 (Ganapathy 2013).
For many years neurocritical care was considered to be essentially a part of the neurosurgical ICU or neurosurgical recovery room, with well-established protocols for managing such patients. It is believed that there may be 100 to 125 neurosurgical ICUs in India, but the distribution of these centres may not be uniform. For example, Chennai, a city in the southern part of India, has a population of nine million people with 110 neurosurgeons, which is also the number of neurosurgeons catering to 250 million people in North Eastern India.
Head Trauma
About 40 per cent of all deaths in India are still due to infections.
The majority of the remainder is mainly due to non-communicable conditions. 11%
of deaths in India from non-communicable diseases are due to injuries, of which
78% of injury deaths are due to road traffic accidents. Road traffic injuries
are the leading cause (60%) of traumatic brain injury (TBI), followed by falls
(20%-25%) and violence (10%). The World Health Organization (WHO) has projected
that by 2020 road crashes will be a major killer in India, accounting for
546,000 deaths (Peden 2004). The only epidemiological study undertaken in
Bangalore at the National Institute of Mental Health and Neurosciences
(NIHMANS) has revealed that the incidence, mortality and case fatality rates
were 150/1,00,000, 20/1,00,000 and 10%, respectively. NIMHANS provides care for
nearly 60-70% of brain-injured persons in Bangalore city. 7,164 persons were
enrolled into a Neurotrauma Registry during the year 2000 at NIMHANS (Gururaj
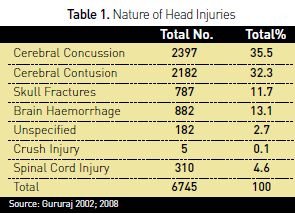
2002). The nature of head Injuries in this registry is shown in Table 1.
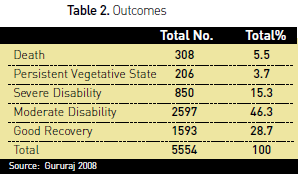
Information on duration of hospital stay was available for 5554 (82%) of the subjects. The outcomes of these patients are reflected in Table 2.
Due to the lack of adequate emergency medical services patients reach
hospital late; this has a major impact on outcomes. At least one-third of
potentially preventable deaths occur prior to arrival at hospital, and over
half occur during the hospital reception and resuscitation phase of care. Over
80% of accident victims do not achieve access to medical care within one hour
of the incident. A study from Mumbai noted that for severely injured patients,
the time between the injury and hospital admission averaged 6 hours (Murlidhar
and Roy 2004).
Stroke
There are eight stroke registries based in various states of India. Each
registry independently set up its stroke surveillance systems, based on the WHO
STEPS guidelines (http://www.who.int/chp/steps/en/). The Indian Council of Medical
Research (ICMR) initiated several strategies to integrate the registries and
develop a common population-based stroke registry for the country, but it is
still under development (WHO 2006). Some registries are trying to conduct
feasibility studies that would help establish this common population-based registry
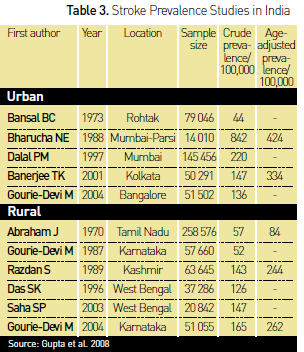
for stroke patients. Based on these registry data the prevalence of stroke is
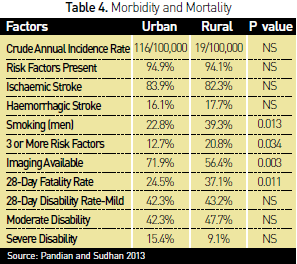
illustrated in Table 3. Table 4 demonstrates the morbidity and mortality from
the Trivandrum registry.
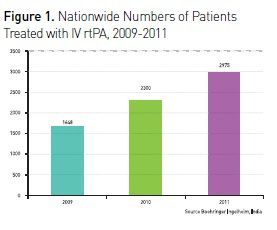
The proportion of stroke patients reaching hospital within three hours in India is 15%. This is due to the unavailability of emergency ambulance services, especially in rural areas (Ghandehari 2011). In our web-based Indian Critical Care discussion group survey, to the question how many critical care physicians thrombolysed acute is chaemic stroke, as per the NINDS rt-PA study protocol (National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group 1995), of the 126 respondents 49 (38.89%) responded positively, and of these 11 (8.73%) also used intra-arterial thrombolysis performed by an interventional radiologist.
Despite a high prevalence of stroke in India, the number of stroke patients receiving recombinant tissue plasminogen activator (rtPA), as in other third world countries, is extremely low (Ghandehari 2011). Some of the most important barriers for thrombolysis in India are pre-hospital barriers, financial constraints and lack of Infrastructure.
There is a lack of knowledge about stroke thrombolysis among medical professionals. A study by Nandigam and colleagues (2003) demonstrated that a significant majority of general physicians in India are not aware of the beneficial effects of tissue plasminogen activator (tPA). A study from South India reported that 30% of stroke patients reached the hospital within three hours post event and 16% were eligible for thrombolysis therapy, but all of these eligible patients belonged to a lower socioeconomic group and could not afford the therapy due to its high cost (Ghandehari 2011).
Intracerebral haemorrhage (ICH) is associated with high mortality and morbidity. Low Glasgow Coma Scale score, higher baseline ICH volume, presence of intraventricular haemorrhage and need for ventilatory assistance are independent predictors of mortality. In a 2013 study by Bhatia and colleagues, most of the patients with spontaneous ICH were disabled at discharge. Surgery did not improve mortality or outcome.
Stroke-associated early seizures (ES) often complicate the initial course of acute stroke. In a study in Kolkata, of the 441 patients (49.43% had haemorrhagic stroke), 79 (17.91%) suffered from ES. Alcoholism, haemorrhagic stroke, cortical and severe strokes predict development of ES. ES are an independent important risk factor for early mortality (Goswami et al. 2012).
Subarachnoid Haemorrhage (SAH)
Incidence of SAH in Kashmiri, a northern part of India, is high, being
about 13/100,000 persons per year. SAH comprises 31.02% of total strokes and
aneurysmal ruptures are the cause of 54.35% SAHs (Bhat et al. 2011).
In a study by Sharma and colleagues (2011) 168 aneurysms were coiled in 150 patients over a six-year study period. Procedure-related rupture during endovascular coiling occurred in 2.97% of procedures, and was responsible for 1.78% treatment-related deaths. Risk factors were small aneurysm size, previous SAH. The outcome of treatment of aneurysm with coiling is safe (Sharma et al. 2011). Aneurysm surgery is performed extensively in India.
Stroke Units
A stroke unit is a multidisciplinary team comprising medical, nursing,
physiotherapy, occupational therapy, speech therapy, and social work staff. In
India there are approximately 35 stroke units, and they are predominantly in private
sector hospitals in the cities (Pandian and Sudhan 2013). According to the
Mumbai registry study, only 306 of 456 (67.2%) patients with first-ever stroke
were managed at a healthcare facility, and the remaining 150 (32.8%) patients
were cared for at home or in nursing homes (Dalal et al. 2008).
Intracranial Pressure Monitoring (ICP)
ICP monitoring is routinely performed in very few centres in India. This
is probably due to the assumption that ICP monitoring is technologically very
demanding, and also because commercially available systems are extremely
expensive in the Indian setting (Joseph 2003). The intraventricular drain,
which is the most frequently used technique, is cost-effective and has shown a
higher incidence of nosocomial meningitis. The more modern fibre optic devices are
clearly more expensive. In the web survey regarding ICP monitoring and
multimodal monitoring the observation is shown in Figure 2 and Figure 3.
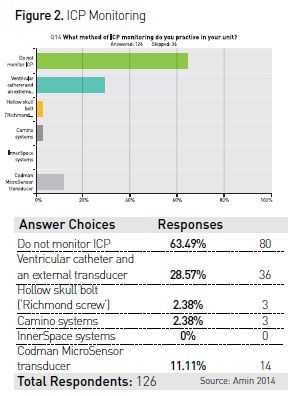
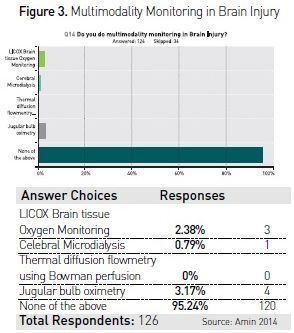
Only 33 (26.19%) critical care consultants of the 126 respondents of the survey had facilities in their units to carry out continuous EEG monitoring in patients suspected to have status epilepticus. 49 respondents of the 126 were regularly doing transcranial Dopplers in their ICUs.
Conclusion
Neurocritical care is a well-established specialty in the developed
world. The success of the speciality is due to integration of various sub-specialities,
namely neurology, neurosurgery, neuro-anaesthesiology, interventional neuroradiology
and neuro-critical care. The phenomenal progress demonstrated by general critical
care in India was due to the contribution of ISCCM in increasing awareness to
the medical community and the public at large. ISCCM over the years conducted
seminars, continuing medical education, workshops, national and international
conferences along with a curriculum to train young potential intensivists. For
neurocritical care to move ahead a similar cohesive group or a subgroup of
ISCCM needs to establish standards of neurocritical care practice and probably
set up a curriculum for a diploma in neurocritical care.
For full references, please email [email protected], visit the website at www.icu-management.orgor use the QR code at the top of the article.




















