Researchers at Tübingen University have developed a new technique to safely mark T-cells for non-invasive in vivo imaging to better understand what happens during immune reactions in the body. This technique enabled the investigators to track the T-cell movement in mice using positron emission technology (PET). Previous methods used to follow the movement of T-cells by PET impaired or even damaged the cells.
The immune system's T-cells are a key starting point for researchers developing immunotherapies against cancer and autoimmune diseases. T-cells are constantly on the move throughout the body, checking for invading pathogens and diseased cells. If any of these structures which fit the T-cells' specific receptors like a key fits the right lock — then the T-cell will proliferate and set off a series of signals, starting the process of eradicating the diseased cell.
Each T-cell recognises only one specific pattern on the cell's surface and there are thousands of different T-cells. If the T-cells miss their target or if they mistakenly order the destruction of a healthy cell, the result will be disease in the form of infection, cancer, allergies or autoimmune conditions, explain the researchers, led by Professor Bernd Pichler at the Werner Siemens Imaging Center. They describe the new technique in the latest issue of PNAS.
For this study, Professor Pichler and colleagues placed an antibody with a weak radioactive component onto the receptors on the T-cells' outer membrane. This radiation could be seen and measured by the PET device. T-cells constantly recycle the receptors on their outer membrane, transporting them inside the cell — in this case, along with the radioactive marker.
"The blocked T-cell receptor is no longer available to recognise the specific antigen," according to lead author Dr. Christoph Griessinger. "But the specific receptors are quickly resupplied and the immune reaction is barely impaired."
The marker remains stable in the T-cell for about 48 hours, giving the researchers enough time to take their measurements. After that, the radioactive material will be largely decayed and the radiation will be too weak, project leader Dr. Manfred Kneilling explains.
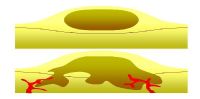
The T-cells' functions are barely hindered despite the marker, and PET technology provides high-contrast images. As such, the researchers were able to watch live coverage of how the T-cells targeted and specifically migrated into infected tissue. Supported by comparative control testing, in which the researchers induced inflammation using very similar antigens not matching the specific T-cell, they were able to prove that T-cells only migrate into tissue inflamed by their specific antigen.
"This technique could be applied to other cell types of the immune system — anywhere the receptors on the membrane are renewed often," Dr. Griessinger points out. There are already plans to apply the technique in humans, he adds.
Imaging techniques, the researchers note, are becoming ever more important in the fields of cellular immunotherapy and stem-cell transplantation. For instance, imaging could be used in new cancer treatments in which the patient's own immune system is employed to target tumour cells. "We would be able to mark the treated immune cells as we did the T-cells and to track whether they migrate to the tumours as planned," Dr. Kneilling adds.
Source: Universitaet Tübingen
Image Credit: Flickr.com
The immune system's T-cells are a key starting point for researchers developing immunotherapies against cancer and autoimmune diseases. T-cells are constantly on the move throughout the body, checking for invading pathogens and diseased cells. If any of these structures which fit the T-cells' specific receptors like a key fits the right lock — then the T-cell will proliferate and set off a series of signals, starting the process of eradicating the diseased cell.
Each T-cell recognises only one specific pattern on the cell's surface and there are thousands of different T-cells. If the T-cells miss their target or if they mistakenly order the destruction of a healthy cell, the result will be disease in the form of infection, cancer, allergies or autoimmune conditions, explain the researchers, led by Professor Bernd Pichler at the Werner Siemens Imaging Center. They describe the new technique in the latest issue of PNAS.
For this study, Professor Pichler and colleagues placed an antibody with a weak radioactive component onto the receptors on the T-cells' outer membrane. This radiation could be seen and measured by the PET device. T-cells constantly recycle the receptors on their outer membrane, transporting them inside the cell — in this case, along with the radioactive marker.
"The blocked T-cell receptor is no longer available to recognise the specific antigen," according to lead author Dr. Christoph Griessinger. "But the specific receptors are quickly resupplied and the immune reaction is barely impaired."
The marker remains stable in the T-cell for about 48 hours, giving the researchers enough time to take their measurements. After that, the radioactive material will be largely decayed and the radiation will be too weak, project leader Dr. Manfred Kneilling explains.
The T-cells' functions are barely hindered despite the marker, and PET technology provides high-contrast images. As such, the researchers were able to watch live coverage of how the T-cells targeted and specifically migrated into infected tissue. Supported by comparative control testing, in which the researchers induced inflammation using very similar antigens not matching the specific T-cell, they were able to prove that T-cells only migrate into tissue inflamed by their specific antigen.
"This technique could be applied to other cell types of the immune system — anywhere the receptors on the membrane are renewed often," Dr. Griessinger points out. There are already plans to apply the technique in humans, he adds.
Imaging techniques, the researchers note, are becoming ever more important in the fields of cellular immunotherapy and stem-cell transplantation. For instance, imaging could be used in new cancer treatments in which the patient's own immune system is employed to target tumour cells. "We would be able to mark the treated immune cells as we did the T-cells and to track whether they migrate to the tumours as planned," Dr. Kneilling adds.
Source: Universitaet Tübingen
Image Credit: Flickr.com
References:
Griessinger CM, Maurer A, Kesenheimer C et al. (2015) 64Cu antibody-targeting of the T-cell receptor and subsequent internalization enables in vivo tracking of lymphocytes by PET. Proceedings of the
National Academy of Sciences, 2015; 201418391 DOI:
10.1073/pnas.1418391112
Latest Articles
Cancer, Infections, PET, immunotherapy, immune system, T-cell
Researchers at Tübingen University have developed a new technique to safely mark T-cells for non-invasive in vivo imaging to better understand what happen...