Experienced emergency medicine doctors shared their thoughts on leadership in several sessions at the European Society of Emergency Medicine congress in Glasgow last week.
Ruth Brown, consultant in emergency medicine, Imperial College Healthcare NHS Trust, London, UK spoke about emerging leadership. She reasoned that leaders need experience and self-confidence. They need to have seen many patients, build confidence in those learning to lead, have a positive outlook, have vision (a plan), be flexible, motivate, and focus on people. Leaders should have emotional intelligence, which includes self-awareness, self-regulation, social skills and empathy.
Brown acknowledged that enculturation happens when students go to medical school This entails a loss of idealism, ritualised professional identity, emotional neutralisation, and a change of ethical integrity. Enculturation is balanced by learning the less formal aspect of "the good EM practitioner". The leadership element of hidden curriculum is very important.
Fostering and developing one’s own and others’ leadership skills requires thought and deliberate practice, Brown emphasised: “Be the leader you want others to be.”
When you're faced with conflict involve colleagues in the circle of patient care and advocate for your patient. For example, when talking to radiology about a scan request: “I'm sure you can understand the implications of both of us missing this diagnosis'.”
Carr emphasised that emergency medicine doctors are paid to make decisions, and quoted Peter Rosen, Emeritus Professor of Emergency Medicine at the University of California, San Diego: “I think the worst emergency physician is one that can’t make a decision. It may not be the right decision. You might have to change it. But you can’t stand and dither.”
People can be uncivil and rude in all walks of life, but did you know that it affects performance? Chris Turner, an emergency medicine consultant University Hospitals Coventry & Warwickshire, and co-founder of Civility Saves Lives, explained why civility saves lives. The shame of having someone be rude to you closes you down. The impact of mild to moderate rudeness reduces cognitive ability in the moment by 61%. How we behave towards each other is the single greatest factor in how well competent teams perform. Incivility also has an impact on staff onlookers—a 20% decrease in performance and a 50% reduction in willingness to help others. The impact on patients and relatives is 75% less enthusiasm for the organisation. 66% feel anxious dealing with employees.
He quoted Matt Scanlon, PICU doc, Milwaukee: “The difference between work-as-done and work-as-imagined is critical because ‘standard practice’, policies and rules are often premised on work-as-imagined and thus unrealistic, untenable and completely unworkable.’
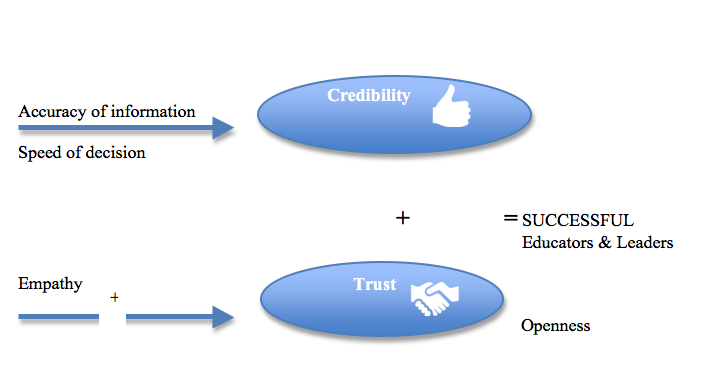
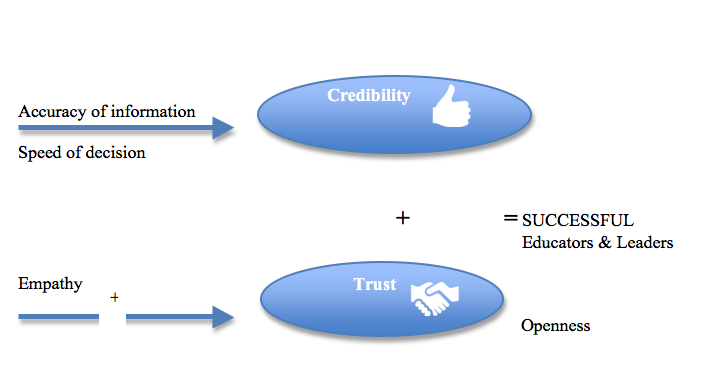
Norms, values, and beliefs can shape the future of our specialty, according to Aristomenis Exadaktylos, Professor of Emergency Medicine, University Hospital Bern, Switzerland, who shared a formula for successful educators and leaders:
Group members discuss as peers critically and support the decision of the group, even it might not be their personal choice and remain openly critical (this helps later in debriefings).
He quoted Norman Schwarzkopf, the United States Army general: “Leadership is a potent combination of strategy and character. But if you must be without one, be without the strategy.”
Ruth Brown, consultant in emergency medicine, Imperial College Healthcare NHS Trust, London, UK spoke about emerging leadership. She reasoned that leaders need experience and self-confidence. They need to have seen many patients, build confidence in those learning to lead, have a positive outlook, have vision (a plan), be flexible, motivate, and focus on people. Leaders should have emotional intelligence, which includes self-awareness, self-regulation, social skills and empathy.
Brown acknowledged that enculturation happens when students go to medical school This entails a loss of idealism, ritualised professional identity, emotional neutralisation, and a change of ethical integrity. Enculturation is balanced by learning the less formal aspect of "the good EM practitioner". The leadership element of hidden curriculum is very important.
Fostering and developing one’s own and others’ leadership skills requires thought and deliberate practice, Brown emphasised: “Be the leader you want others to be.”
Philosophy of emergency medicine
From Canada, David Carr, an emergency physician at University Health Network in Toronto, shared his philosophy of emergency medicine:- Don't be afraid to say 'I don't know'
- Know how to shift gears when department gets bus
- Keep tabs on your learners
- Think about flow - use your time wisely
- Get home on time, it's the route out of burnout.
When you're faced with conflict involve colleagues in the circle of patient care and advocate for your patient. For example, when talking to radiology about a scan request: “I'm sure you can understand the implications of both of us missing this diagnosis'.”
Carr emphasised that emergency medicine doctors are paid to make decisions, and quoted Peter Rosen, Emeritus Professor of Emergency Medicine at the University of California, San Diego: “I think the worst emergency physician is one that can’t make a decision. It may not be the right decision. You might have to change it. But you can’t stand and dither.”
Rudeness makes us less / civility saves lives
People can be uncivil and rude in all walks of life, but did you know that it affects performance? Chris Turner, an emergency medicine consultant University Hospitals Coventry & Warwickshire, and co-founder of Civility Saves Lives, explained why civility saves lives. The shame of having someone be rude to you closes you down. The impact of mild to moderate rudeness reduces cognitive ability in the moment by 61%. How we behave towards each other is the single greatest factor in how well competent teams perform. Incivility also has an impact on staff onlookers—a 20% decrease in performance and a 50% reduction in willingness to help others. The impact on patients and relatives is 75% less enthusiasm for the organisation. 66% feel anxious dealing with employees.
Neil Spenceley spoke about playing nicely in the sandbox. He advised walking in others shoes, such as a nurse, cleaner or nurse. He reinforced Chris Turner’s points about incivility: “disrespect is a threat to patient safety because it inhibits collegiality and cooperation…cuts off communication and undermines morale.” “Disrespectful behaviour is ….learned, tolerated, and reinforced in the hierarchical hospital culture” (Leape et al. 2012 free fulltext available). Invivility leads to a blame culture in an organisation, which as we know is detrimental to clinical safety.
He quoted Matt Scanlon, PICU doc, Milwaukee: “The difference between work-as-done and work-as-imagined is critical because ‘standard practice’, policies and rules are often premised on work-as-imagined and thus unrealistic, untenable and completely unworkable.’
Norms, values, and beliefs can shape the future of our specialty, according to Aristomenis Exadaktylos, Professor of Emergency Medicine, University Hospital Bern, Switzerland, who shared a formula for successful educators and leaders:
Group members discuss as peers critically and support the decision of the group, even it might not be their personal choice and remain openly critical (this helps later in debriefings).
Tips for achieving consensus
- Avoid win-lose techniques
- Do not encourage harmony as an objective
- Don’t intimidate others
He quoted Norman Schwarzkopf, the United States Army general: “Leadership is a potent combination of strategy and character. But if you must be without one, be without the strategy.”
References:
Klingberg K, Gadelhak K, Jegerlehner SN, Brown AD, Exadaktylos AK, Srivastava DS (2018) Bad manners in the Emergency Department: Incivility among doctors. PLoS One, 13(3):e0194933.
Latest Articles
Leadership, rudeness, emergency medicine, European Society of Emergency Medicine, #EuSEM18, incivility
Experienced emergency medicine doctors shared their thoughts on leadership in several sessions at the European Society of Emergency Medicine congress in Glasgow last week.
























