As medicine transitions to high-value practice, there is more urgency to obtain the most diagnostically accurate information possible from each CT examination while protecting patients from unnecessary scans, radiation, and costs. Body CT is a leading source of patient radiation exposure in medical imaging, and imagers must embrace the pledge to safeguard patients by optimising radiation use put forth by the Image Wisely Campaign, says a review article in the Journal of American College of Radiology.
In body CT, radiation dose is tempered by limiting the number of phases performed during each CT and modulating tube current and peak kilovoltage. The ACR recently released their second slate of Choosing Wisely recommendations, which advises radiologists to avoid abdominal CT protocols with noncontrast and delayed phases unless the additional acquisitions provide an incremental increase in valuable diagnostic information.
Reduction of CT dose can compromise image quality and confound diagnosis by increasing noise, which has been addressed by manufacturers developing iterative reconstruction, notes the journal article.
"Radiologists may not be aware of additional resources available at the scanner and the workstation to increase lesion conspicuity and detection as image quality and quantity decrease, including virtual noncontrast data sets from dual-energy CT, 3D rendering (maximum intensity projection [MIP], volume rendering [VR], and cinematic rendering [CR]),
computer-assisted diagnosis, and texture analysis," the article explains.
The utility of a virtual nonenhanced scan for improving diagnostic performance is best demonstrated in patients with gastrointestinal haemorrhage, the article says. Although the diagnosis can be made without an unenhanced scan, by identifying intraluminal contrast extravasation that changes configuration between arterial and venous phases, addition of a virtual noncontrast data set increases diagnostic confidence.
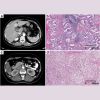
Meanwhile, use of MIP renderings at the workstation can improve detection of lung nodules and renal calculi on noncontrast scans performed with low-dose techniques. "For contrast-enhanced scans, MIP renderings increase conspicuity of small hypervascular hepatic metastases (such as neuroendocrine tumour) on the arterial phase scan," the article explains. "MIP rendering of arterial phase data sets aids in characterisation of solitary hepatic masses by confirming neovascularity in malignant tumours and depicting the classic feeding artery in focal nodular hyperplasia."
As dose reduction increases noise, 3D rendering becomes increasingly important because, as the article points out, the postprocessed images maintain diagnostic quality to a greater extent than axial source images. Notably, this tool can help guide the management of oncology patients, including determination of pancreatic cancer resectability and renal cell carcinoma operative planning.
"Innovations such as texture mapping and CR are equally important, because they advance management guidance and further poise radiologists to serve as valuable members of the patient care team," according to the article published by Pamela T. Johnson, MD, and Elliot K. Fishman, MD, both with Johns Hopkins Radiology in Baltimore, Maryland.
Source: Journal of American College of Radiology
Image Credit: Pixabay
References:
Johnson PT, Fishman EK (2018) Enhancing Image Quality in the Era of Radiation Dose Reduction: Postprocessing Techniques for Body CT. J Am Coll Radiol. March 2018 15:3/Part A 486–488 https://doi.org/10.1016/j.jacr.2017.11.001
Latest Articles
CT Imaging, Body CT, low-dose techniques, patient radiation exposure
As medicine transitions to high-value practice, there is more urgency to obtain the most diagnostically accurate information possible from each CT examination while protecting patients from unnecessary scans, radiation, and costs.