HealthManagement, Volume 17 - Issue 5, 2017
Improving the radiological image
Prof. Rui Almeida gives an analysis on his research which was applied to general radiology exams.
The main goal of this research was to assess the effect of an internal and participative intervention aimed through the implementation of best practices and quality improvement applied to general radiology exams. Therefore, a quality improvement cycle was conducted in a radiology department considering a total of 5 criteria and 13 sub-criteria of quality assessment. At baseline, 11 of the criteria/sub-criteria presented quality failures but during the revaluation the improvements were significant in 8 of the criteria/subcriteria. So, the internal quality assessment cycle has been useful and effective as a routine tool for continuous quality improvement of the healthcare process.
The access to healthcare services has increased worldwide, but the quality of care provided to the patients still is a global health challenge (Scott et al. 2014). In this context, an imaging department (public or private), has a great importance in a networked organisational structure, since its contribution to the clinical diagnosis is crucial in most cases (Macedo and Rodrigues 2009; Almeida et al. 2010). Thus, the need to provide better healthcare services to patients goes through the implementation of quality management programmes, defined as "the set of structural elements and activities which specific purpose is the continuous quality improvement" (Saturno 2008; Juran et al. 1990).
Three main starting points can be identified in quality management programmes aiming the continuous quality improvement of the radiology departments, in particular, 1) quality improvement cycles, 2) quality monitoring and 3) quality planning (Saturno 2008; Palmer 1990). In the specific case of quality improvement cycles, they start with the identification of an opportunity for improvement (quality problem) in some aspect of the offered services, with the purpose of "taking advantage" of the opportunity to improve or "solve" the identified problem (Saturno 2008; Juran et al. 1990; Figueiredo and Gama 2012).
The quality of the product/service provided in a radiology department consists on "obtaining precise/ accurate diagnostic information with the lowest dose of exposure to all hazardous factors that is reasonably achievable and at a minimal, realistic cost." (Erturk et al. 2005). So, repeat exposures should be avoided due to poor image quality, because it increases the risks to the patient and the costs to the department, and, at the same time, can reduce t he accuracy of image interpretation, and may even result in dissatisfaction among patients, workers and the institution itself (Erturk et al. 2005; Felício and Rodrigues 2010).
General radiology procedures continue to be the one with the highest number of examinations performed worldwide (around 3.6 billion examinations per year) and is expected to continue to increase due to the introduction of new digital technologies and the increase in the number of equipment (UNS CEAR 2008; Teles et al. 2012). Thus, we should have a concern with the quality of this procedures, especially with the image quality and the technical parameters, through their optimisation, since they influence the quality and also the patient safety.
Therefore, considering that the general strategic lines of a radiology department must ensure processes that correspond to the patient needs, performed according to the best available scientific evidence, and to develop a culture of continuous improvement through teamwork and the involvement of all department stakeholders, the present study consisted in evaluating the effect of an internal and participative intervention to implement the best practices and improve the quality applied to general radiology examinations. In order to achieve this goal, a quality improvement cycle directed to the radiological image was carried out in order to maximise its quality based on criteria and interventions defined by the radiographers themselves.
Materials and methods:
Based on a quality improvement cycle with a quasi-experimental design before-after, following the SQUIRE (Standards for Quality Improvement Reporting Excellence) guidelines, six sequential methodological steps were developed in a public radiology department in Portugal (Taylor et al. 2013; Portela et al. 2015):
- Identification and prioritisation of the quality problem: 6 radiographers
performed a qualitative analysis using the nominal group technique adapted with
two other techniques: 1) brainstorming on the possible problems and 2) preliminary
and final voting using a prioritisation matrix focused on the following
criteria: problem frequency, gravity, dependence on internal efforts to solve
it and solution costs. The quality of general radiology exams was prioritised.
- Analysis of the problem causes: A cause-andeffect diagram and a qualitative
analysis of all potential causes of the prioritised problem were performed.
This study was focused only on the measurement of the causes in which there was
scientific evidence of its relation to the problem and that would allow to
develop criteria and indicators to measure quality.
- Development of quality criteria: A group of 4 experts in the radiology field
developed a list of quality criteria and sub-criteria related to the image
quality of general radiology, using a format that included its definitions,
exceptions and clarifications. Face, content and criterion-related validity were
analysed and considered adequate for all the criteria. Moreover, through a
pilot study and using a sample of 30 exams and 2 independent evaluators, all
criteria were identified with consistent reliability (general agreement
observed above 95% for all criteria).
- Evaluation of the quality level: Systematic random samples and convenience
samples (n=60) were used considering a total of 5 criteria and 13 subcriteria of
quality assessment. Data were collected using different data sources according
to the analysed criteria. The initiative of the evaluation was decided by the
radiographers (internal evaluation), in which they were responsible for the
data collection, performing a cross-evaluation.
- Quality improvement intervention: It was based on a structured and
participatory planning method. The ideas generated to answer what should be done
to improve the quality of general radiology examinations allowed to distribute,
through an affinity diagram, four main groups of actions to be implemented: 1)
Radiographers training on "dosimetry and technical parameters to be used
according to the anatomical region under study" and "image
post-processing”, 2) Physicians training on “national and international
legislation about the principles of Justification, Optimisation and Dose
Limitation” in relation to the prescription of radiological examinations, which
should contain adequate clinical information so that radiographers can
evaluate, programme and perform these examinations according to the patients
clinical situation, in order to obtain the best diagnostic images, 3)
Organisation of work procedures and establishment of standards related to image
postprocessing and 4) Dissemination of the study results through the
elaboration of a storyboard (with the inclusion of the activities progress and awareness-raising
actions to monitor the results). After establishing these actions, a Gantt
diagram was used to supervise their implementation.
- Revaluation of the quality level: 18 weeks after the improvement intervention
and 24 months after the initial evaluation, a new quality level evaluation was
carried out based on the same assumptions expressed in step 5.
Results
Initial evaluation of the quality level
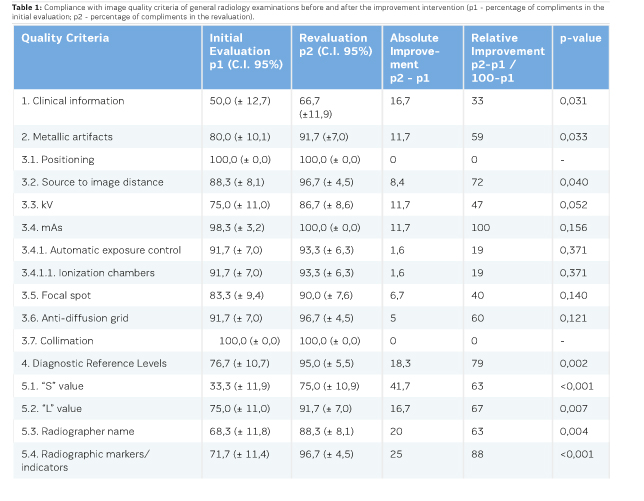
The level of compliance with the quality criteria under study was evaluated for a confidence level of 95% (Table 1) and it was observed that the percentages of compliance in the initial assessment were between 33.3% and 100%. The quality criteria with the highest levels of compliance were the following: "(3.1) Positioning of the patient and the anatomical region under study" and "(3.7) Collimation", both with 100%, and "(3.4) mAs" with 98.3% (C.I 95%, 95.1-100). On the other hand, the quality criteria with the lowest levels of compliance were: "(5.1) Adequacy of the “S” value", "(1) The radiological examination prescribed by the physician should contain adequate clinical information regarding the anatomical region under study" and “(5.3) Inclusion of the initial letters of the name and surname of the radiographer” with compliance rates of 33.3% (C.I. 95%, 21.4-45.2), 50.0% (C.I. 95%, 37.3 -62.7) and 68.3% (C.I. 95%, 56.5-80.1), respectively.
Analysis of quality defects and intervention prioritisation
A Pareto diagram was constructed according to the initial evaluation data, where it was possible to identify the most problematic quality criteria, called "vital few from the trivial many" according to the "Pareto principle". Thus, in the initial evaluation, 4 quality criteria (5.1, 1, 5.3 and 5.4), which together represented 60.92% of the total defects found, were considered as priorities in the actions/interventions to be established to improve quality.
Revaluation of the quality level
After completing the quality improvement intervention plan, there were improvements (absolute and relative) in all quality criteria that had defects in the initial evaluation.
The minimum relative improvement was 19% for quality sub-criteria "(3.4.1) Automatic Exposure Control" and "(3.4.1.1) Ionisation Chambers", and maximum for the sub-criteria "(4) Diagnostic reference levels", "(5.4) Radiographic Markers/Indicators" and "(3.4) mAs" with 79%, 88% and 100%, respectively.
It was found that improvements in quality levels were statistically significant (p <0.05) in eight of the criteria and sub-criteria. Considering that two of the quality criteria already had 100% of compliance in the initial evaluation, this represents a significant improvement in more than half of the total criteria evaluated.
Considering these data and those in the initial evaluation, it was possible to construct the before-after Pareto graph (Figure 1), where we can observe and compare the values of the defects in the two evaluations performed. It was possible to verify that quality criteria 1, 5.1, 3.3 and 5.3 represented 66.67% of the noncompliance cases verified in the re-evaluation. Thus, in a new intervention planning, these should be the main criteria to be considered in establishing the actions and tasks to be performed, not neglecting all others that still presented defects.
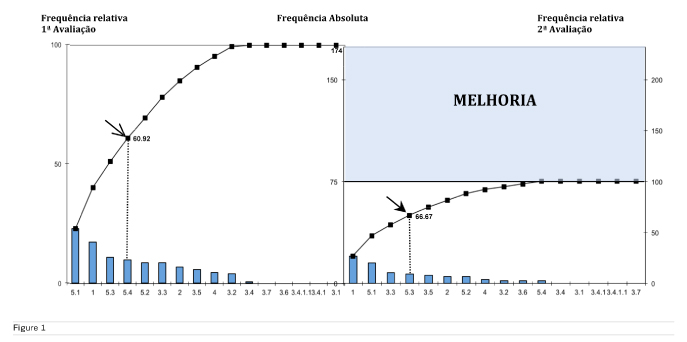
Through Table 1 and Figure 1, we can also observe that the total of quality failures decreased from 174 in the initial evaluation to 75 in the revaluation, which corresponds to an absolute improvement of about 43% (marked improvement area in the Pareto graph).
It was verified for the four quality criteria on which the improvement activities were most important during the intervention, statistically significant improvements ranging from 33% to 88%.
Conclusion
Although the use of quality improvement cycle in healthcare services is still rudimentary, especially in the radiology departments, the quality criteria based on scientific evidences and the results obtained by assessing their level of compliance, before and after intervention, demonstrated that the internal quality improvement cycle was useful to ensure better image quality through optimised and safer procedures.
Despite the fact that quality culture is still not properly incorporated in the analysed department, the use of this participatory method allowed to open doors to the implementation of quality management internal activities, with the inclusion of all stakeholders. A quality problem has been prioritised, which should continue to be the target of the evaluation cycle, but many others are identified and can be now analysed using the same methodology since the improvements were evident and most of them significant.
The rational intervention, based on data from an evaluation of valid and reliable quality criteria, the voluntary accountability of radiographers, and the audit and feedback of partial results, proved to be useful to improve significantly the quality of this healthcare service.
The development of evidence-based quality criteria has contributed to the improvement achieved, and the fact that the image quality is now higher has contributed to an increase in patient safety by reducing repeat examinations and more favourable conditions for performing better diagnostic imaging.
Despite the good results obtained, the improvement margin is still great. From the four quality criteria on which improvement activities were most pronounced during the intervention, three of them remain the most problematic criteria after re-evaluation, which can be explained in several ways. On the one hand, the other quality criteria have low levels of defects and, therefore, the margin for improvement is much lower. On the other hand, the resistance to change and the technical- scientific knowledge of some radiographers may have influenced the improvement of these criteria, which still have a good margin of progression.
Due to the great variability processes into a radiology department, caution is necessary in extrapolating the results of the levels of compliance with the quality criteria of this study to other services. However, regarding the effectiveness of the quality improvement cycle method, consistent statistical significance has proven to be a very promising, useful and effective approach for improving the image quality problem of general radiology exams, which will certainly bring benefits to other departments.
Key Points
- The
implementation of quality management programme is defined as "the set of
structural elements and activities specific purpose is the continuous quality
improvement"
- Strategic
actions of a radiology department must ensure processes that correspond to the
patient needs performed according to the best available scientific evidence
- In
this study, the minimum relative improvement was 19% for the quality sub-criteria
“Automatic exposure control” and “Ionisation chambers”, and maximum for the
sub-criteria “Radiographic markers/indicators” and “mAs” with 88% and 100%,
respectively
- Absolute
frequency of quality failures decreased from 174 (baseline) to 75 (revaluation)
- The
internal quality assessment cycle has been useful and effective as a routine
tool for continuous quality
- improvement
of the healthcare process
References:
Almeida RP, Silva CA, Fernandes RA, et al. (2010). Manual da Qualidade e Abordagem por processos: O caso de uma sala de Mamografia. TMQ (Techniques, Methodologies and Quality) – A Qualidade numa perspectiva multi e interdisciplinar – Qualidade e Saúde: perspectivas e práticas, 1:157-174. Lisboa: Sílabo.
Erturk SM, Ondategui-Parra S, Ros PR (2005). Quality Management in Radiology: Historical Aspects and Basic Definitions. J Am Coll Radiol. 2:985-991.
Felício CM, Rodrigues VM (2010). A adaptação do técnico de radiologia às novas tecnologias. Radiologia Brasileira, 43(1):23-28.
Figueiredo FM, Gama ZA (2012). Melhoria da proteção radiológica mediante um ciclo de avaliação interna da qualidade. Radiologia Brasileira, 45(2):87-92.
Juran JM, Gryna FM, Bringhan RS (1990). Manual de control de la calidad. 2ª ed. Barcelona: Reverté. Macedo HE, Rodrigues VM (2009). Programa de controle de qualidade: a visão do técnico de radiologia. Radiologia Brasileira, 42(1):37-41.
Palmer RH (1990). Evaluación de la assistencia ambulatoria. Principios y práctica. Madrid: Ministerio de Sanidad y Consumo.
Portela MC, Pronovost PJ, Woodcock T, et al. (2015). How to study improvement interventions: a brief overview of possible study types. BMJ Quality & Safety, 0:1-12. doi:10.1136/bmjqs-2014-003620
Saturno PJ (2008). Gestión de la calidad. Concepto y componentes de um programa de gestión de la calidad. Manual del máster en gestión de la calidad en los servicios de salud. Módulo 1: Conceptos básicos. Unidad temática 2. 2ªed. Murcia: Universidad de Murcia.
Scott KW, Phil M, Jha AK (2004). Putting Quality on the Global Health Agenda. New England Journal of Medicine, 371:3-5. doi: 10.1056/NEJMp1402157
Taylor MJ, McNicholas C, Nicolay C, et al. (2013). Systematic review of the application of the plan-do-studyact method to improv quality in healthcare. BMJ Quality & Safety, 0:1-9. doi:10.1136/bmjqs-2013-001862
Teles P, Sousa MC, Paulo G, et al. (2012). Relatório sobre os resultados do projecto Dose Datamed 2 Portugal. Avaliação da Exposição da População Portuguesa a Radiação Ionizante devido a Exames Médicos de Radiodiagnóstico e Medicina Nuclear. Sacavém: Instituto Tecnológico Nuclear; 2012. Available from: http://www. itn.pt/projs/ddm2-portugal/Relatorio_Dose_Datamed2_ Portugal.pdf
UNSCEAR (2008). Sources and Effects of Ionizing Radiation. United Nations Scientific Committee on the Effects of Atomic Radiation: Report to the General Assembly with Scientific Annexes. New York: United Nations; 2010. Available from: http://www.unscear.org/ docs/reports/2008/09-




















