The classic model of a boss, or someone in charge, focusing on command-control, using the style of rewarding or punishing subordinates, has generated an anachronistic experience in managing human capital while building an environment of psychological security, collaboration, and innovation.
These are currently fundamental in the healthcare space.
In the past, the healthcare leaders were often physicians, as examples of charismatic and entrepreneurial leadership, while in the public sector, experienced managers alongside medical doctors led the institutions.
In the last five decades, healthcare has been an area where rising costs, accelerating demographic and epidemiological changes, and the attraction of private investors have led to immense transformations. In particular, the patient has moved from a "passive" position to a more individual and pro-active role (Patrnchak 2015).
The role of the executive and care leaders, as well as of the clinical care "support" sectors, has shifted in health institutions, from mostly financial to focusing on patient safety concerns.
In 2010, ANAHP (National Association of Private Hospitals) discussed the importance of developing medical and clinical staff management leadership as indispensable for delivering excellent care and delivering value to the patient and the health system.
In the intervening decade-plus it led to at least three integration leadership models such as:
(i) transformational healthcare leadership;
(ii) servant leadership in healthcare (dual-layer model);
(iii) digital leadership, for tackling current health scenarios. (accelerated in the COVID-19 pandemic) (Trastek 2014).
This pandemic has further established the Digital Leader by flattening governance structures, increasing the relevance of optimising safety practices, paying increasing attention to the physical and mental health of their team members, managing and making data-driven decisions, and tolerating highly uncertain environments (Constancio et al 2014) .
Traditional Business and Management schools, in their M.B.A. programmes, have always looked at the healthcare executive leader as the other market leaders - entrepreneurs, i.e., with a strong emphasis on managerial competencies, implementing strategic planning, maximising profit, and focusing on operational efficiency and a culture of customer satisfaction. However, health care has seen a profound shift in the priorities of this leadership style in order to deliver high-value care from the formation and development of its high-performance teams (Cosgrove 2014; Fraher & Fried 2018).
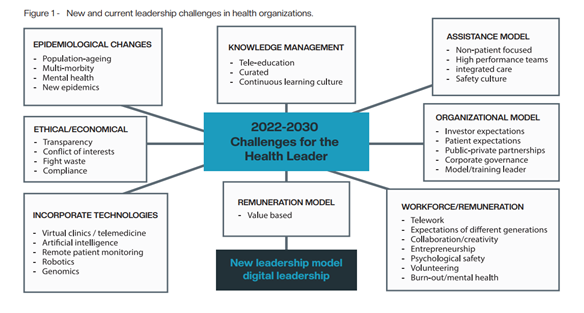
This new scenario has promoted changes in the governance of organisations with boards of directors, professionalisation, and the prioritisation of developing their leaders through institutional programs to train better leaders for the "new times" (Fig.1). The English National Health System (NHS) is an excellent example of this in requiring a full training of its workforce via a digital transformation (Topol 2019).
Despite echoing this movement and need, health care in Brazil is a sector that remains predominantly ANALOG and the resultant numerous difficulties, evident on a daily basis.
Brazilian healthcare is in dire need of implementing the electronic medical record and electronic exchange of patient information, for example, particularly in the face of the intense and rapid changes inherent to digital transformation.
The Brazilian College of Health Executives - CBEXs survey identified in 2021 that for 74% of leaders, the pandemic accelerated the digital transformations in their organisations.
This new leadership model, while still under construction, has as its mission to foster the discussion about the powerful combination between the protagonism and influence of managers and leaders, the digital assets of organisations, and the development of people as a strategy to achieve faster efficiency, sustainability, and the desired economic impact in healthcare organisations, all in the context of transformation and improvement.
Managing these assets creates value for the patient by working with data, building new information and knowledge for the institution and the Healthcare chain4. Therefore, the digital leader must become immersed in the culture, understand and relate to start-ups, implement agile methodologies, learn to react quickly and adequately to all healthcare environment changes.
The "new patient" (called 4.0) has access to their health care information, the patient 4.0 is also accelerating changes on the path to transforming healthcare services. Understanding these new and growing demands becomes critical to acquiring and retaining your customers. The digital patient journey thus starts to be built and be monitored, removing rework by the institution's professionals and the feeling of lost time or institutional disorganisation by the patient (Constancio et al. 2021)
Digital leadership, therefore, is a model under development that will allow for training new leaders, and represents a set of competencies or capabilities that seeks to accelerate the desired transformations. Incorporating these new attributes via both digital assets of people and organisations aims at seeking better outcomes, reduction of adverse events, lower costs, providing a unique patient experience, and facilitating better access and expanding communication between the health care professionals. Digital assets!
These digital assets are defined as all the (digital) components of an organisation that generate value for customers and employees, as well as profitability for shareholders. These include relationship strategy, content, data and information generation, services and products from or through digital technologies.
Properly nurturing and managing these assets expands the touch points (communication links, relevant information, reliable data...) has the ability to increase interaction between organisation, employees, and customers, consolidates the brand, and goes beyond the geographic reach and variety of service and product offerings, whether digital in part or as a whole.
In addition, agile management and problem solving methodologies will be increasingly deployed to improve individual projects and speed up transformations and the decision making of leaders. This model also involves supporting innovation in the work context, developing an environment towards the mindset of exponential growth, offering mentoring and growth practices to people at the top, so to capture creative solutions in an open and collaborative way (Constancio et al 2021).
Seen in this light, it becomes mandatory for the current leader to lead people through the language of the world of information technology and communication, the internet, innovations and applications.
This leader must also understand and know how to identify and apply the best use of these technological tools in the daily operation of the institution, aiming at improving performance and productivity, efficiency in decisions and the strategic alignment of daily activities to the business objectives (Topol 2019). The development of these new skills and competencies are thus essential.
A set of skills and competencies are very important for the digital leader in healthcare, which have been consolidated in different publications (Constancio et al 2021).
1. Visionary with an exponential growth mindset - The digital leader, from a well-defined and well understood purpose, has the ability to foresee evolving scenarios, spot new business possibilities, and list solutions to complex problems with this digital and exponential way of thinking.
2. Connected Learner - Digital leaders must have a thirst for learning and relearning what brings results and impacts people's lives in this landscape. They invest their time in connecting with mentors, innovative communities, and are active users of digital tools that allow them to develop the necessary skills.
3. Facilitator and Mentor – needs to understand that knowledge and information are distributed throughout an organisation in a horizontal, not top down fashion, needing control and facilitation to be structured in a parallel fashion.
4. Creative and Designer - Digital leaders realize they can design and create new projects never before imagined because of the limitations of the analog and face-to-face world. They invest their time in thinking about and designing the delivery of a future in the digital age.
5. Efficient and data-driven - Understanding that in the digital age efficiency goes hand in hand with the use of data is the first step. Digital leadership bases its actions on data and hard facts that are generated by efficient structuring of its operation. However, at no time does it ignore human experience and intuition.
6. Incorporates agile methodologies for innovation - The digital leader impacts how new ideas are developed, then validated into prototypes of minimal viability and launched into the marketplace. Rapid and less costly experimentation, based on continuous learning, allows innovation to be viewed in a lighter and more compelling way.
7. Focused on the needs, behaviors and "pains" of patients and their networks - In the digital age, it is customer networks that drive change, not mass markets anymore. Customers dynamically connect and interact, changing relationships with each other and with companies: they discover, evaluate, comment, use products and services through digital tools.
8. Obsession with data security and privacy - The way companies generate, store and process information is different in the digital age. Big data and artificial intelligence tools provide the reasons for companies to predict and anticipate both undesired and positive scenarios and patterns. As a result, the obsession with broadly maintaining the security of this personal and/or sensitive information is unprecedented as a result of large-scale leaks, theft, and misuse.
Thus, for Brazilian healthcare this analog to digital transformation presents a great opportunity and adapting this new model of a digital leader. It needs to use data science and artificial intelligence to improve processes, increase predictive capacity, and incorporate agile methodologies in projects and in the search for solutions to organisational problems.
References:
1. Patrnchak JM (2015). Implementing servant leadership at Cleveland Clinic: a case study in organizational change. Servant Leadership: Theory & Practice. 2(1): 36-48.
2. U.S. News Best Hospitals (2018) Cleveland Clinic. Available from: http://health.usnews.com/best-hospitals/area/oh/cleveland-clinic-6410670/rankings.
3. Trastek VF, Hamilton NW, Niles EE (2014) Leadership models in health care - a case for servant leadership. Mayo Clinic Proceedings. 89(3): 374-381.
4. Constancio IT. Siqueira I. Balestrin F (2021) Manual do Gestor Hospitalar - Federação Brasileira de Hospitais. Digital Leadership in Health. 98-109. Brasília.
5. Cosgrove, T (2014) The Cleveland Clinic Way: Lessons in Excellence from One of the World's Leading Health Care Organizations. Ed. McGraw Hill; 1st edition.
6. Fraher EP, Fried Bi (2018) Health-care workforce. In: Chronic Illness Care: Principles and Practice. New York, NY: Springer International Publishing. 527-536.
7. Topol E (2019). Preparing the healthcare workforce to deliver the digital future Internet. NHS Health Education England. Available from: https://topol.hee.nhs.uk/wp-content/uploads/HEE-Topol-Review-2019.pdf