HealthManagement, Volume 15, Issue 2/2013
the latter having autonomous status.
Finland is divided into 415 self-governing municipalities (in 2008) with a median number of inhabitants of 5000. Municipalities are autonomous and they are responsible for providing basic services for their residents, including primary education and social and health services. The highest decision-making body in the municipality is the municipal council, which is elected
by general election every four years. Municipalities levy a municipal income tax, the rate being decided independently by each municipality. Municipalities also receive some other tax revenues (real estate tax and part of the corporate tax), subsidies paid by the state and other revenues (such as user-fees).
Finnish Health Policy
The key objectives of health policy in Finland are to:- Reduce premature deaths;
- Extend people’s active and healthy life,
- Ensure the best possible quality of life for all; and
- Reduce differences in health.
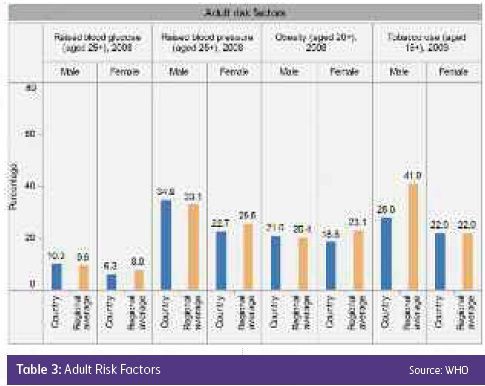
Currently the most significant public health problems include circulatory diseases, malignant tumours, musculoskeletal diseases and mental health problems. Emerging problems are obesity, chronic lung diseases and diabetes (particularly
type 2 diabetes).
Dual Public Financing
There are three different healthcare systems in Finland that receive public funding: municipal, private and occupational healthcare. There are significant differences between the systems, for example in the scope of the services provided, user-fees and waiting times. There are also different public financing mechanisms for healthcare services in Finland: municipal financing based on taxes and National Health Insurance (NHI) financing based on compulsory insurance fees.Municipalities fund municipal healthcare services (except outpatient drugs and transport costs) and NHI funds for example private healthcare, occupational healthcare, outpatient drugs, transport costs, sickness allowances and maternity leave allowances. This dual public financing creates challenges for the overall efficiency of service production, particularly in pharmaceutical care where dual financing incurs cost-shifting problems.
Municipalities
The largest share of publicly financed healthcare is provided by the municipal healthcare system (71% of outpatient physician visits, 59% of outpatient dentists visits and 95% of inpatient care periods). According to legislation, more than 400 municipalities are responsible for providing all necessary health services for their residents. Municipalities have a significantdegree of freedom to plan and steer the services as they see best, and state level steering could be described as weak.
There have been many local development projects and experiments concerning municipal services aimed at increasing cooperation between municipalities, between primary and secondary care services and between municipalities and the
private sector. However, they are not well coordinated from the national level, which has caused regional variance in structures.
It could be said that public responsibility for healthcare is more decentralised in Finland than any other European country and some believe the problems outweigh the advantages. However, there are signs that the decentralisation trend has slightly reversed and national level steering will increase. For example, the governmental programme for the restructuring of municipalities and services has a goal to decrease the number of municipalities and increase cooperation between
municipalities.
According to legislation, every municipality must have a health centre which provides primary health services. Additionally, legislation divides the country into 20 hospital districts (excluding Åland islands), which are responsible for the provision
of municipal secondary care services. Each municipality must be a member of one hospital district. Hospital districts are financed and managed by the member municipalities. Often municipalities experience a lack of influence on the volume and costs of the hospital districts, despite the fact that they directly own them, and find that primary healthcare is in too weak a position relative to secondary healthcare.
Legislation sets maximum user-fees and an annual ceiling for healthcare charges for municipal services. These user-fees cover on average 7% of municipal healthcare expenditure. Outpatient drugs are not covered by the municipal healthcare system, but by NHI instead. On average, 67% of outpatient drug costs are reimbursed to the patient. There is a (separate) ceiling for out-of-pocket payments for outpatient drugs. Both the municipal healthcare and outpatient drugs ceilings are high compared with other Nordic countries. In extreme situations social assistance is available (when an individual’s or a family’s income is not enough to cover the user-fees of municipal healthcare services or outpatient drugs).
National Health Insurance Scheme
The statutory NHI scheme finances 17% of the total costs of healthcare. The scheme is run by the Social Insurance Institution (SII), with about 260 local offices all over the country. SII falls under the authority of the Parliament and covers all Finnish residents. NHI is funded by the insured (38%), employers (33%) and the state (28%). The insured pay income-based insurance fees which are collected alongside taxation.The use of private healthcare is partly reimbursed by NHI. The private sector provides about 16% of outpatient visits to physicians, 41% of outpatient visits to dentists and 5% of inpatient care periods. NHI covers about one third of the actual costs of the private health services. Additional voluntary health insurance is not widespread in the Finnish healthcare system
and is mainly used to supplement the reimbursement rate of NHI.
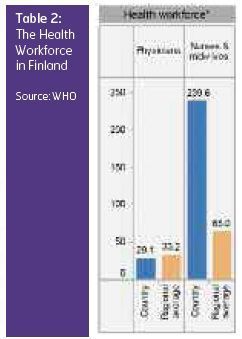
Health Workforce
The majority of physicians work for municipalities and hospital districts. Physicians in health centres and hospital districts are usually salaried employees of the municipalities. However, during the last 10 years a new trend has emerged to lease the physician workforce to health centres from private firms. Eleven per cent of physicians have a private practice as a full-time job and 30% work full-time in the public sector but hold a private practice outside their regular working hours.Since the late 1990s there has been a significant shortage of physicians in Finland, which has had a significant impact on the developments of the healthcare system. In order to rectify this situation the yearly intake of medical students has been increased considerably.
Important Reforms
The most important state level reforms from the beginning of the 1990s have been:- Deregulation of state steering of municipal health services and related changes in state administration (1993);
- National Project to Ensure the Future of Health Care (2002–2007);
- Extension of public dental health care to all age groups (2002);
- Introduction of the waiting time guarantee (2005);
- Project to restructure municipalities and services (ongoing since 2005); and
- Development of the national electronic patient record system (ongoing since 2006).
In addition, there have been several reforms concerning pharmaceuticals, with one important goal being to further promote cost containment. In terms of the distribution of benefits, there are two major challenges in the Finnish healthcare system: geographical inequities and inequities between socioeconomic groups. There are significant differences between municipalities
in service provision (for example in physician visits, dental care, mental healthcare, elective surgery) and waiting times. There are also significant differences between municipalities in resources invested in municipal healthcare leading to differences in the quality and scope of municipal services. However, these inequalities can also partly be explained by other differences
between municipalities such as age structure, morbidity rates and use of private and occupational healthcare services.
There are also significant socioeconomic inequalities in the use of healthcare services. Among OECD countries pro-rich inequity in physician visits was found to be one of the highest in Finland (along with the United States and Portugal) in 2000. Significant pro-rich differences are also evident in screening, dental care, coronary revascularizations and in some elective specialised care operations (hysterectomy, prostatectomy and lumbar disc operations). Although overall mortality has fallen, the socioeconomic inequality in mortality seems to be increasing.
Conclusion
The Finnish healthcare system offers relatively good quality health services for reasonable cost with quite high public satisfaction. The most visible problems are long waiting times and personnel shortage in some municipalities. An ageingpopulation, new medical technology, drug innovations and increasing population expectations will create challenges for the Finnish healthcare system in the near future. There are also some structures in the Finnish healthcare system which are perceived as problematic: the level of decentralisation, poor steering capacity in the system, relatively weak position of primary care, a lack of cooperation between primary and secondary care and dual financing.
Text adapted from:
Vuorenkoski L, Mladovsky P and Mossialos E. Finland:
Health system review. Health Systems in Transition. 2008; 10(4): 1–168.