Smartphone technology acceptable for telemedicine and stroke
A Mayo Clinic study has validated the use of smartphones medical images to evaluate stroke patients in remote locations. The study tested the effectiveness of smartphone teleradiology applications in a real-world telestroke network.
"Essentially what this means is that telemedicine can fit in our pockets," says Bart Demaerschalk, M.D., professor of Neurology, and medical director of Mayo Clinic Telestroke. "For patients this means access to expertise in a timely fashion when they need it most, no matter what emergency room they may find themselves."
Mayo Clinic pioneered clinical research to study telemedicine to serve patients with stroke in non-urban settings. Today, Mayo Clinic is the hub in a network of 12 other spoke centres, all but one in Arizona. In telestroke care, the use of telemedicine platforms or robots located in a rural hospital lets a stroke patient be seen in real time by a neurology specialist who typically is working from a desktop or laptop computer in Phoenix. The Mayo Clinic stroke neurologist, whose face appears on a computer screen, consults with emergency room physicians at the rural sites and evaluates the patient.
Patients showing signs of stroke can be examined by the neurologist who can also view scans of the patient's brain to detect possible damage from a hemorrhage or blocked artery. If necessary patients can be administered clot-busting medications within the narrow window of time necessary to minimise permanent injury to the brain.
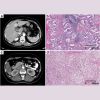
This study compared the quality of medical images using a particular smartphone application to the same types of information and images typically viewed via desktop computers. Mayo Clinic neurologists worked with emergency physicians and radiologists at Yuma Regional Medical Center to compare brain scan images from 53 patients who came to that medical centre with stroke.
The scans were reviewed by radiologists in Yuma and a separate adjudication panel of stroke neurologists to determine the level of agreement between these traditional interpretation routes and new images and scans on smartphones interpreted by telestroke doctors. The study shows there was a high level of agreement (92 to 100 percent) among all the reviewers over the most important radiological features.
"Smartphones are everywhere," Dr. Demaerschalk says. "If we can transmit health information securely and simultaneously use the video conferencing capabilities for clinical assessments, we can have telemedicine anywhere, which is essential in a state like Arizona where more than 40 percent of the population doesn't have access to immediate neurologic care."
Mayo Clinic Hospital in Phoenix is conducting a pilot adoption of ResolutionMD Mobile on the iPad and iPhone among physicians and surgeons in the departments of radiology, neuroradiology, neurology, neurosurgery, orthopedics, and transplants, he said.
Image and Diagnosis Quality of X-Ray Image Transmission via Cell Phone Camera: A Project Study Evaluating Quality and Reliability
Researchers in Bonn, Germany examined several paramaters for assessment of x-ray images, which had been photographed and transmitted via cell phone.
A total of 100 x-ray images of various body regions were photographed with a Nokia cell phone and transmitted via email or MMS. The transmitted photographs were reviewed on a laptop computer by five medical specialists and assessed regarding quality and diagnosis.
Due to their poor quality, the transmitted MMS images could not be evaluated and this path of transmission was therefore excluded. Mean size of transmitted x-ray email images was 394 kB (range: 265-590 kB, SD ±59), average transmission time was 3.29 min ±8 (CI 95%: 1.7-4.9). Applying a score from 1-10 (very poor - excellent), mean image quality was 5.8. In 83.2±4% (mean value ± SD) of cases (median 82; 80-89%), there was agreement between final diagnosis and assessment by the five medical experts who had received the images. However, there was a markedly low concurrence ratio in the thoracic area and in pediatric injuries.
While the rate of accurate diagnosis and indication for surgery was high with a concurrence ratio of 83%, considerable differences existed between the assessed regions, with lowest values for thoracic images. Teleradiology is a cost-effective, rapid method which can be applied wherever wireless cell phone reception is available. In our opinion, this method is in principle suitable for clinical use, enabling the physician on duty to agree on appropriate measures with colleagues located elsewhere via x-ray image transmission on a cell phone.