Breast density remains a hot topic in radiology, and although much is known about the impact of breast density on mammographic screening, what to do with that information is not always clear. Polarisation
of opinion on the pros and cons of mammographic screening has left
women confused, and hindered early detection of breast cancer, according to Professor Murray Rebner, Immediate Past President, Society of Breast Imaging. HealthManagement.org spoke to Prof. Rebner in advance of his presentation at the EUSOBI Annual Scientific Meeting next month on “Dense breasts: Implications for the patient and the radiologist.”
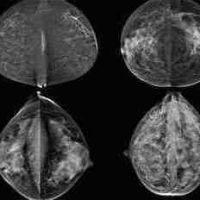
Legislation to inform women about their breast density is now in place in many states in the USA. Are primary care doctors, radiologists and women well informed about the issue?
I think that most primary care doctors and women in the United States have, at best, a rudimentary understanding of the issue of breast density. They have learned that increased density makes it harder to interpret a mammogram, but they probably do not know what to do with the information.
Radiologists are far more likely to be aware of the implications of breast density since they are the ones who decide what density type is associated with a patient’s breasts. They are the ones who should have access to the woman’s personal and family risk factors for breast cancer, and they may suggest that the patient undergo a risk assessment evaluation, consult with a genetic counsellor or receive supplemental screening.
Is enough known about breast density and breast cancer risk?
We are discovering more about breast density and breast cancer risk, but we still need to learn more. For example, it is now clear that stromal cells in the tumuor microenvironment play an important role in cancer development. If the mechanism of this “cross-talk” could be better defined, then specific inhibitor agents might be developed to arrest the process. Also, is there a critical mass of stromal tissue which is needed for this to occur? If yes, accurate breast density measurements would take on greater importance. Finally, are there genetic mutations which impart a high risk of breast cancer development that are also associated with increased breast stromal content?
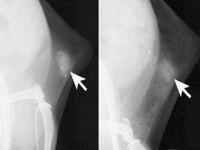
Tomosynthesis is now reimbursed by the Centers for Medicare and Medicaid Services in the USA. Do you foresee that tomosynthesis will become the most prevalent screening technology or where there still be a role for MRI and ultrasound for certain risk groups?
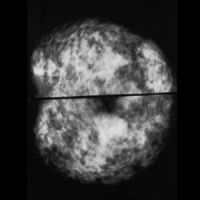
It is apparent that we have entered the era of personalised breast cancer screening. I believe that tomosynthesis will eventually replace standard digital mammography (DM) as the primary breast cancer screening tool. Studies to date have shown that it detects more curable, invasive breast cancers in women of all breast densities, and it also lowers recall rates for women with different breast densities compared to standard DM. Supplementary screening (in addition to mammography, not as a replacement for mammography) with MRI and ultrasound is becoming more widespread. Combining MRI with mammography to screen women at high risk for breast cancer increases sensitivity by almost threefold; however, the specificity typically remains lower compared to mammography. In women with dense breasts, screening with automated ultrasound combined with mammography can detect an additional two cancers per thousand women screened; however the specificity is less than mammography alone. MRI screening usage has increased over time; however, ultrasound screening has not been widely utilised by the American radiology community. The time to perform and interpret the studies are barriers to its acceptance. Abbreviated breast MRI screening may ultimately prove to be the supplementary screening modality of choice.
Would you like to comment on the polarisation of opinion on the pros and cons of mammographic screening?
I believe that the polarisation of opinion on the pros and cons of mammographic screening has left women confused, and has hindered our ability to detect breast cancer at its earliest point of development. Unfortunately, the science of breast cancer screening is not straightforward. Organisations such as the Society of Breast Imaging and the American College of Radiology are trying to present the facts in a clear, intelligible fashion. What is clear is that mammography saves lives. Since the 1980s, when mammography utilisation became widespread in the United States, breast cancer mortality has decreased by 30%. Population-based screening programmes in Sweden, the Netherlands and Norway have shown similar mortality reductions. Panels such as the United States Preventive Services Task Force have members who do not treat breast cancer patients and have no expertise in breast cancer screening. However, they are making a value judgment that the harms of mammography outweigh its benefits. Also, the issue of overdiagnosis is overstated. It is not in the 20-50% range as purported by some authors; when all the correct variables are accounted for it is less than 10% and the majority of the cases represent non-invasive tumors. The media is also at fault. They are quick to report on the anti-screening publications; however, we almost never see coverage of papers which demonstrate a benefit from early detection by screening. Women should have discussions about breast cancer screening with their healthcare providers and they should make informed decisions about their own health care. However, in order to do this, they and their healthcare providers need to have accurate, evidence-based information at their disposal. We are working hard to provide the facts.
Claire Pillar
Managing editor
HealthManagement.org
Legislation to inform women about their breast density is now in place in many states in the USA. Are primary care doctors, radiologists and women well informed about the issue?
I think that most primary care doctors and women in the United States have, at best, a rudimentary understanding of the issue of breast density. They have learned that increased density makes it harder to interpret a mammogram, but they probably do not know what to do with the information.
Radiologists are far more likely to be aware of the implications of breast density since they are the ones who decide what density type is associated with a patient’s breasts. They are the ones who should have access to the woman’s personal and family risk factors for breast cancer, and they may suggest that the patient undergo a risk assessment evaluation, consult with a genetic counsellor or receive supplemental screening.
Is enough known about breast density and breast cancer risk?
We are discovering more about breast density and breast cancer risk, but we still need to learn more. For example, it is now clear that stromal cells in the tumuor microenvironment play an important role in cancer development. If the mechanism of this “cross-talk” could be better defined, then specific inhibitor agents might be developed to arrest the process. Also, is there a critical mass of stromal tissue which is needed for this to occur? If yes, accurate breast density measurements would take on greater importance. Finally, are there genetic mutations which impart a high risk of breast cancer development that are also associated with increased breast stromal content?
Tomosynthesis is now reimbursed by the Centers for Medicare and Medicaid Services in the USA. Do you foresee that tomosynthesis will become the most prevalent screening technology or where there still be a role for MRI and ultrasound for certain risk groups?
It is apparent that we have entered the era of personalised breast cancer screening. I believe that tomosynthesis will eventually replace standard digital mammography (DM) as the primary breast cancer screening tool. Studies to date have shown that it detects more curable, invasive breast cancers in women of all breast densities, and it also lowers recall rates for women with different breast densities compared to standard DM. Supplementary screening (in addition to mammography, not as a replacement for mammography) with MRI and ultrasound is becoming more widespread. Combining MRI with mammography to screen women at high risk for breast cancer increases sensitivity by almost threefold; however, the specificity typically remains lower compared to mammography. In women with dense breasts, screening with automated ultrasound combined with mammography can detect an additional two cancers per thousand women screened; however the specificity is less than mammography alone. MRI screening usage has increased over time; however, ultrasound screening has not been widely utilised by the American radiology community. The time to perform and interpret the studies are barriers to its acceptance. Abbreviated breast MRI screening may ultimately prove to be the supplementary screening modality of choice.
Would you like to comment on the polarisation of opinion on the pros and cons of mammographic screening?
I believe that the polarisation of opinion on the pros and cons of mammographic screening has left women confused, and has hindered our ability to detect breast cancer at its earliest point of development. Unfortunately, the science of breast cancer screening is not straightforward. Organisations such as the Society of Breast Imaging and the American College of Radiology are trying to present the facts in a clear, intelligible fashion. What is clear is that mammography saves lives. Since the 1980s, when mammography utilisation became widespread in the United States, breast cancer mortality has decreased by 30%. Population-based screening programmes in Sweden, the Netherlands and Norway have shown similar mortality reductions. Panels such as the United States Preventive Services Task Force have members who do not treat breast cancer patients and have no expertise in breast cancer screening. However, they are making a value judgment that the harms of mammography outweigh its benefits. Also, the issue of overdiagnosis is overstated. It is not in the 20-50% range as purported by some authors; when all the correct variables are accounted for it is less than 10% and the majority of the cases represent non-invasive tumors. The media is also at fault. They are quick to report on the anti-screening publications; however, we almost never see coverage of papers which demonstrate a benefit from early detection by screening. Women should have discussions about breast cancer screening with their healthcare providers and they should make informed decisions about their own health care. However, in order to do this, they and their healthcare providers need to have accurate, evidence-based information at their disposal. We are working hard to provide the facts.
Claire Pillar
Managing editor
HealthManagement.org
References:
Latest Articles
Breast density, Mammographic screening, tomosynthesis
Interview with Professor Murray Rebner about breast density and breast cancer risk, tomosynthesis and his presentation at EUSOBI 2015 annual scientific meeting