A Mayo Clinic study shows that molecular breast imaging (MBI) for women with dense breast tissue resulted in a lower cost per cancer detected than screening with mammography alone. MBI helped increase accuracy of breast cancer diagnosis, and in combination with mammography, resulted in cost savings of approximately 15 percent, according to the new study published in the American Journal of Roentgenology (AJR).
The MBI technology known as LumaGEM®, developed and commercialised by Gamma Medica, Inc., is a cost-effective tool for detecting early stage cancers in women who have dense breast tissue. "The [Mayo Clinic study] results reinforce the importance of LumaGEM and accelerate our pace to bring the advanced MBI technology to radiologists searching for more accurate tools to diagnose breast cancer," said Philip Croxford, President and CEO of Gamma Medica. "In addition to the results, which support MBI's promise as a safe, cost-effective, supplemental screening alternative for those with dense breast tissue, women found it to be an easy and comfortable experience."
Early detection of breast cancer through screening remains the most reliable method to manage the disease. However, for women with dense breast — which accounts for 45 percent of all women — traditional screening methods lack the clarity and accuracy to detect early stage cancers.
An additional publication of the Mayo Clinic study in the AJR concluded there was a four-fold increase in detection rates as compared with standard mammography when using LumaGEM as a secondary screening method. Unlike mammography, tomosynthesis and ultrasound — all of which are anatomical imaging tests — the LumaGEM system is a functional imaging modality that highlights the metabolic activity in the breast regardless of tissue density. This allows radiologists to clearly identify early stage cancers. MBI provides equivalent sensitivity, and improved specificity, when compared to magnetic resonance imaging (MRI), but at roughly one-third of the cost.
"These publications emphasise the value of MBI with a safe low-dose capability, a lower cost per cancer detected and a higher detection rate of breast cancer malignancy that isn't achievable by other breast imaging modalities," said Scott Headland, Gamma Medica's Vice President of Sales. "This study underscores the need for Gamma Medica to hasten every effort in growing the adoption of LumaGEM MBI for all women with dense breast tissue."
Source: Gamma Medica, Inc.
Image credit: American Journal of Roentgenology
The MBI technology known as LumaGEM®, developed and commercialised by Gamma Medica, Inc., is a cost-effective tool for detecting early stage cancers in women who have dense breast tissue. "The [Mayo Clinic study] results reinforce the importance of LumaGEM and accelerate our pace to bring the advanced MBI technology to radiologists searching for more accurate tools to diagnose breast cancer," said Philip Croxford, President and CEO of Gamma Medica. "In addition to the results, which support MBI's promise as a safe, cost-effective, supplemental screening alternative for those with dense breast tissue, women found it to be an easy and comfortable experience."
Early detection of breast cancer through screening remains the most reliable method to manage the disease. However, for women with dense breast — which accounts for 45 percent of all women — traditional screening methods lack the clarity and accuracy to detect early stage cancers.
An additional publication of the Mayo Clinic study in the AJR concluded there was a four-fold increase in detection rates as compared with standard mammography when using LumaGEM as a secondary screening method. Unlike mammography, tomosynthesis and ultrasound — all of which are anatomical imaging tests — the LumaGEM system is a functional imaging modality that highlights the metabolic activity in the breast regardless of tissue density. This allows radiologists to clearly identify early stage cancers. MBI provides equivalent sensitivity, and improved specificity, when compared to magnetic resonance imaging (MRI), but at roughly one-third of the cost.
"These publications emphasise the value of MBI with a safe low-dose capability, a lower cost per cancer detected and a higher detection rate of breast cancer malignancy that isn't achievable by other breast imaging modalities," said Scott Headland, Gamma Medica's Vice President of Sales. "This study underscores the need for Gamma Medica to hasten every effort in growing the adoption of LumaGEM MBI for all women with dense breast tissue."
* * * * * * * *
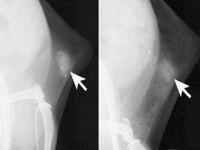
Small molecular breast imaging (MBI)-occult invasive ductal carcinoma detected by mammography in 49-year-old woman. (A) Left craniocaudal image from digital screening mammography was interpreted as showing focal asymmetry in lower inner left breast (arrow) that was less conspicuous on diagnostic evaluation and was recommended for short-interval follow-up in six months, at which time biopsy was performed. (B) Adjunct craniocaudal image from MBI obtained at time of screening mammography was interpreted as negative. Final pathology was 0.3-cm grade II invasive ductal carcinoma.Top image
Source: Gamma Medica, Inc.
Image credit: American Journal of Roentgenology
References:
Hruska CB et al.(2015) Diagnostic workup and costs of a single supplemental molecular breast imaging screen of mammographically dense breasts. AJR Am J Roentgenol. 2015 Jun;204(6):1345-53. doi:
10.2214/AJR.14.13306
Rhodes DJ et al. (2015) Journal club: molecular breast imaging at reduced radiation dose for supplemental screening in mammographically dense breasts. AJR Am J Roentgenol. 2015 Feb;204(2):241-51. doi: 10.2214/AJR.14.13357
Rhodes DJ et al. (2015) Journal club: molecular breast imaging at reduced radiation dose for supplemental screening in mammographically dense breasts. AJR Am J Roentgenol. 2015 Feb;204(2):241-51. doi: 10.2214/AJR.14.13357
Latest Articles
healthmanagement, Gamma Medica, breast cancer, dense breasts, LumaGEM
A Mayo Clinic study shows that molecular breast imaging (MBI) for women with dense breast tissue resulted in a lower cost per cancer detected than screening with mammography alone.