The US Preventive Services Task Force (USPSTF) has declined to expand its recommendations on which women should receive regular mammography screening. It has instead issued a draft of new screening guidelines that are tilted towards its conservative guidance from 2009.
Similar to the 2009 recommendations, the new guidelines advise that women in their 50s only need a mammography screening every two years. This is in contrast with the annual screening that is advocated by several women's health, oncology and radiology groups. The new guidelines also stop short of recommending screening for women in their 40s on the grounds that the benefits of such a screening do not outweigh the harms associated with it.
The USPSTF claims that it has analysed the evidence from randomised controlled trials and drew the same conclusions that were reached in 2009. These include:
- Mammography benefits
for women at average breast cancer risk will come from biennial screening
between the ages of 50 to 74 years. The highest benefit will go to women aged
60 to 69.
- Screening mammography
for women aged 40 to 49 may reduce mortality but the number of deaths that
could possibly be averted is much smaller than in older women. Also, the number
of false-positive exams and unnecessary biopsies will be much higher. Therefore,
to be screened or not to be screened at this age should be an individual
decision.
- Screening for women
aged 40 to 49 may be beneficial for women with a family history of breast
cancer.
- Women who receive
regular screening mammography are at risk for over-diagnosis.
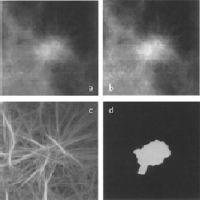
- There is insufficient evidence
to assess the balance of benefit and harms for the use of digital breast
tomosynthesis. Same is true for digital breast tomosynthesis, ultrasound and
MRI for women with dense breast tissue and a negative screening mammogram.
The new guidelines have been severely criticised by mammography advocates. Adoption of these new guidelines could cost thousands of lives and may strip millions of mammography insurance coverage. According to data from the National Cancer Institute, US breast cancer death rate has dropped by 35 percent since mammography screening became widespread in the mid-1980s. Insurance coverage has played a role in this dramatic reduction. Analysis indicates that if women aged 40-49 go unscreened, and women aged 50-74 are screened biennially, approximately 6,500 additional women could die from breast cancer in the US each year.
“The USPSTF limited its consideration to studies that underestimate the lifesaving benefit of regular screening and greatly inflate over-diagnosis claims. They ignored more modern studies that have shown much greater benefit. These limitations result in the misrepresentation of the real trade-offs that women and health care providers need to know about in order to make good decisions about screening. They also ignored the demonstrated views of American women on screening. Unfortunately, these recommendations will only add to confusion that is placing women at risk,” said Barbara Monsees, MD, FACR, chair of the American College of Radiology Breast Imaging Commission.
Source: USPSTF, ACR
Image Credit: CBS News