HealthManagement, Volume 7 - Issue 3, 2007
The Evolving Story
Author
Dr Giles Roditi
Consultant Radiologist
Glasgow Royal Infirmary
Scotland, UK
What is Nephrogenic Systemic Fibrosis?
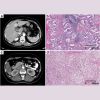
This condition was first described by Dr Shawn Cowper in a paper published in 2000 in The Lancet as a disease with ‘scleromyxoedema-like skin thickening’ affecting the limbs and trunk but typically sparing the face, the first case having been observed in 1997. This new dermatological disease was seen in patients on dialysis and the term nephrogenic fibrosing dermopathy coined to reflect this. Though many systemic diseases that have renal failure as part of their manifestation have dermatological components, no underlying renal disorder linked these patients.
The condition was later renamed nephrogenic systemic fibrosis once it was determined that the fibrosing condition also affects internal organs such as muscles, heart, liver, pleura etc. Some patients only manifest localised non-progressive skin thickening/induration though this can be quite problematic if it interferes with dialysis shunt access. In other patients a progressive disease can be fatal, with contractures due to skin thickening adjacent to joints and terminal illness through the development of a hypostatic pneumonia, particularly when there is diaphragmatic involvement.
The Use of Gadolinium Contrast Agents in Renal
Failure
Gadolinium contrast agents (Gd-CA) have been designed to bind the potentially toxic Gd+++ cation with a chelate in a stable non-toxic compound for human MR imaging and the rate of recorded adverse reactions has been extremely low. These agents are predominantly excreted in the urine by glomerular filtration except for gadobenate dimelumine (Multihance) which in small part undergoes 4% hepatobiliary excretion.
Despite this, is was thought that gadolinium contrast agents for MRI were safe in patients with renal impairment given their high stability and there are studies supporting this. The advent of contrast enhanced MRA (CE-MRA) techniques expanded the use of gadolinium contrast in patients with chronic kidney disease, to investigate the cause of renal failure using CE-MRA to evaluate for renal arterial disease. Furthermore, patients with renal failure are prone to vascular complications and are particularly at risk for complications of arteriography. Lastly, contrast enhanced MR venography (MRV) techniques are extremely useful for assessment of the venous stenoses and thromboses that complicate central venous access for haemodialysis.
The Gadolinium Contrast Agent Link to NSF
A report published (April, 2006) by Thomas Grobner from Austria linked five cases of NSF in dialysis patients over a period of two years to the use of gadolinium contrast agents for MRA in the 2 – 4 weeks preceding the onset of the disease. There was initially some confusion as this paper indicated the agent used to be gadolinium DTPA, however, an erratum was quickly published when it turned out that it was in fact gadolinium DTPA-BMA, otherwise known as gadodiamide (Omniscan, GE Healthcare). A second publication by Marckmann & Thomsen with colleagues from Denmark described thirteen cases of NSF (confirmed on biopsy) and again temporally related the cases to gadodiamide administration between 2 and 75 days prior to disease development.
On the basis of these cases, the FDA in the US issued an advisory in June 2006 urging caution in the use of gadolinium contrast agents in patients with severe renal impairment, i.e. a glomerular filtration rate of less than 15 ml/minute which is classed as chronic kidney disease (CKD) stage 5. This triggered our group to independently study the renal dialysis population in the west of Scotland as a retrospective case control series. For this, we cross-referenced the electronic patient record database for all dialysis patients with the radiology information system to determine NSF incidence and all exposures of these patients to MRI contrast agents.
Findings of our Study
We found the incidence of NSF to be 0.77% of all patients on dialysis and 3.1% of the subgroup of these patients who had undergone gadolinium contrastenhanced MRI. One of the patients with NSF had not had any gadolinium contrast. We also found a positive correlation between the total cumulative dose of Gd-
CA administered and the development of NSF – indicating a form of dose-response relationship, i.e. those patients exposed to higher doses or repeat examinations were more likely to develop NSF.
All the NSF patients in our group who had been exposed to Gd-CA had had gadodiamide, though this was the predominant agent used in the centres at which these patients were imaged and the numbers receiving other agents was too small to draw definite conclusions regarding this. Neither were we able to confirm any other relationships such as with acid-base balance, serum iron etc. within our cohort.
Importantly we note that the majority of our patients in renal failure who have had Gd-CA administered have not developed NSF. Furthermore, we are struck by the very prolonged time between exposure and NSF manifestation in a few of our patients, for example in three patients this was greater than one year which along with our patient with no Gd-CA exposure reinforces our belief that additional factors as yet unknown must play a part in triggering this condition.
How Could Gadolinium Contrast Agents be
Implicated?
The finding of gadolinium in bone biopsy specimens of patients previously administered Gd CA and other work detecting Gd in skin biopsy specimens from NSF patients even many months after exposure, has led to the hypothesis that transmetallation is occurring with Gd+++ being exchanged from the chelate for other cations (e.g. zinc), promoted by the very prolonged time that these agents remain in the body with their primary route of elimination blocked. Toxic-free gadolinium is thought then to stimulate circulating fibrocytes to migrate to the extravascular space and deposit collagen inappropriately resulting in the clinically manifest disease process.
How can We Prevent NSF?
Since renal failure is a prerequisite for the manifestation of this condition it superficially seems simple to just avoid implicated Gd-CA in these patients. However, at what level of renal dysfunction does the risk become a clinical problem? The vast majority of cases of NSF occurred in patients with stage 5 chronic kidney disease (CKD) – i.e. effectively those at the stage of requiring dialysis or established on dialysis. (an estimated glomerular filtration rate (eGFR) of less then 15 ml/min). These patients are easily recognised and can be screened for by the addition of simple questions to pre-MRI checklists. However, if a cut-off of an eGFR of 30 ml/min is required then we need to definitively know the renal function of all our patients prior to MRI examinations and this requires a wholesale change in the way patients are referred for MRI.
The second question is whether it is all contrast MRI studies or only those with high dose administration (0.2 mmol/kg to 0.3 mmol/kg range) that are problematic. Currently it appears that it is high dose studies though unfortunately there are reports of a very few cases after just single dose administration. Hence any policy change currently does not just affect CE-MRA but potentially any MRI examination where Gd-CA may require administeration.
The initial and still the majority of reports of NSF are related to gadodiamide administration, but is this the only agent that should be avoided? Are other Gd-CA more or less likely to predispose this condition? Again there is little to be certain about here, with few cases related to gadoversetamide and gadopentate dimeglumine. There are none confirmed following sole administration of gadobenate dimeglumine and none to date with gadoteridol, gadoterate meglumine, gadobutrol or gadofosveset. However, it is rightly pointed out that these agents have not been as extensively used for high dosage examinations such as CE-MRA.
Some authors feel that transmetallation is an important step in the pathogenesis of NSF and hence there are theoretical reasons why some of these agents would be safer as they are more stable potentially resistant to this process. Cyclic chelates are thought more stable than linear and similarly ionic chelates more stable than non-ionic. The non-ionic linear chelates (such as gadodiamide) are hence thought to be less stable. The potential for hepatobiliary excretion of gadobenate dimelumine may be a theoretical advantage in renal failure and the protein binding of some agents that aids retention in the intravascular space may also be of theoretical benefit though as yet there is no clinical evidence to support these hypotheses.
Dialysis immediately after contrast administration for MRI is theoretically attractive but the role of immediate post-MRI dialysis is uncertain. There is no positive evidence that dialysis can help avert NSF but the current ACR guidelines recommend its use, though this really does need to be immediate post-scan as NSF has occurred in patients despite same day dialysis post- MRI. Clearly dialysis to remove Gd-CA is only practicable where patients already have dialysis access in place prior to MRI.
Other Factors
What other factors are likely to contribute? The studies so far evaluating patients have of necessity been retrospective and therefore uncontrolled. Investigators have searched for other linking factors in these groups such as the nature of the underlying renal disorder, degree of acidosis at time of contrast administration, type of dialysis, erythropoietin treatment, iron levels etc. but so far without any other features being confirmed. The converse of this question as to what factors may protect against the development of NSF has also yet to be answered but could be equally important if ascertained.
Conclusions
The overall implications of the evolving NSF story is that we need to know more about our patients prior to MRI scanning than previously. Renal functional status at the time of scan request for all patients prior to scheduling, particularly for examinations mandating Gd-CA. Additional questions as part of the safety questionnaire prior to MRI scanning.
Where patients with renal failure are considered for MRI with contrast we need to make a judgment as to whether the risks of Gd-CA use as currently perceived outweigh the risks of alternative imaging techniques such as conventional arteriography with arterial puncture, ionising radiation and large volumes of iodinated contrast media.
Where Gd-CA are to be used then the lowest dose feasible is currently advocated (such as half usual dose) and here Gd-CA with increased specific relaxivity could be advantageous. When a scan is planned in a patient with renal failure then clearly close liaison with their renal physician will be required in order to schedule dialysis if this is practicable.
Notwithstanding the evolving NSF story, Gd-CAs remain extremely safe. The finding of a potential connection between Gd-CAs and NSF is a reminder that we must remain vigilant to the safety of all the procedures that we perform, particularly in vulnerable patient groups.