ICU Management & Practice, Volume 19 - Issue 1, 2019
Section Editor Theodorus Kyprianou introduces the “Informatics and Technology” section of ICU Management & Practice.
It is with great pleasure that I introduce today “Informatics and Technology,” an open forum to discuss the role of new, disruptive, hybrid technologies in acute, emergency and intensive care medicine. This brand-new section reflects the vivid interest of the journal’s Editor-in-Chief, in exploring their role in and impact on our everyday clinical practice, teaching and research endeavours, as well as on our managerial and clinical governance decision making processes.
You might also like: Dr. Theodoros Kyprianou joins Editorial Board
The whole medical specialties and healthcare professions spectrum but especially acute care specialties in Europe and the world, face unequivocal challenges and at the same time enjoy unprecedented opportunities amidst the rapidly changing and transformative environment of the 4th industrial revolution (4IR): Cost of Hospital care continues to increase and in 2016, accounted for 32.4 % of the USA’s annual $3.3 trillion health expenditures [of those 38 billion uncompensated!] (CDC.gov; AHA.org) and that of Intensive Care services nearly doubled between 2000 and 2010 ($56 to $108 billion) and as proportion of the Gross Domestic Product increased by 32.1% [0.54% to 0.72% of GDP] (Halpern et al. 2016). Investments in Data, Big Data, analytics and flexible combinations of Internet based tools (what many call as “Internet of things – Internet of everything!”) in healthcare, is projected to grow faster than in manufacturing, financial services, or media, with a compound annual growth rate (CAGR) of 36% through 2025 (Kent 2018). Technology applications that cross the boundaries between physical, digital and biological fields (scientific fields disruption). Game changing dynamics that create opportunities for innovation from small and medium size enterprises and spin-offs and boost individual entrepreneurship outside traditional high-tech regions and countries. Globalisation of personal data and IPRs protection concepts. The following issues, briefly introduced herein set the focus of the new journal section:
(a) Technology enabled, tele-monitoring and remote coordination of healthcare services to acutely and critically ill patients have essentially dissolved the walls fencing traditional acute care areas in hospitals (A&E, ICUs, CCUs, HDUs, post-operative units etc). As a result, there is an ever-increasing demand for numerous forms of acute care -hospital & community based- services, hence for specialised personnel and new, complex clinical routines. At the same time, this highly stressful and complex ICU/HDU routine, demanding career and socially poor life-style, is leading to chronic fatigue/burnout, rendering acute medicine specialties/healthcare professions unattractive to the young generation.
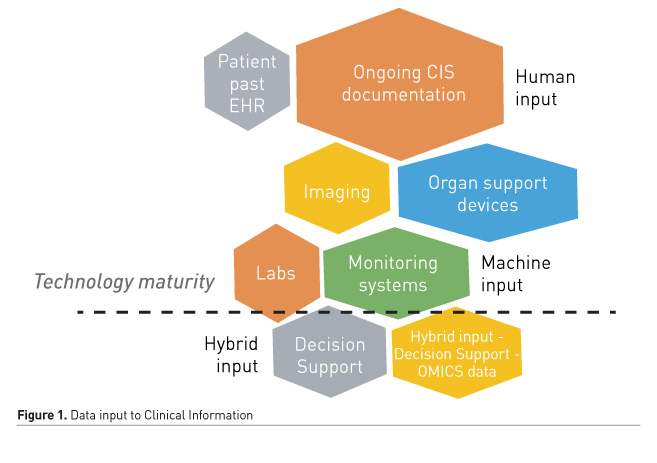
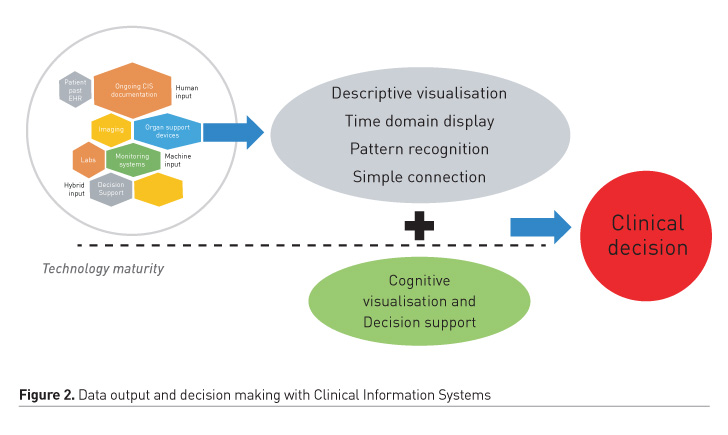
(b) Caring for the acutely/critically ill becomes increasingly complex and encompasses multiple intra-hospital transfers and interactions with numerous medical specialties and healthcare professionals. Hence, it involves 24/7 clinical, administrative and managerial documentation and the use of new biosensors, dynamic imaging methods and ever-increasing organ-specific monitoring systems. It is worth mentioning that there has been an exponential increase of FDA licenses to new medical grade devices and software the last few years [in contrast with the stagnation -in relative terms- in developing new new drugs] (FDA.gov). As a result, a wealth of multiform, structured/unstructured data, clinical biosignals -numeric and waveform- and images is produced (Figure 1), nowadays stored and processed in expense of high storage capacity (ten times more for ICU patients than OR) but decremental cost (Burykin et al. 2011; Blum et al. 2015). However, intuitive visualisation and diagnostic/prognostic use of these data has been increasingly problematic, lacking clinical focus and mostly limited to unguided, experiential, pattern recognition and coding (Evans 2016; Islam et al. 2018; Clifton et al. 2015) (Figure 2).
(d) Failure of the vast majority of randomised studies the last decades -the gold standard of clinical experimentation- to bring positive results in complex critical illness i.e. sepsis (Ridgeon et al. 2016) and traumatic brain injury (Asehnoune et al. 2017), have increased the demand for conceptually personalised approaches to diagnosis and treatment. “Precision Medicine (National Research Council 2011),” reflecting the need to deliver the right treatment at the right time to the right group of persons (encompassing similar characteristics) in the right circumstances! High hopes have been ignited by the fact that the IR4 is bringing to the market -even not yet extensively to the bedside- a whole new spectrum of -omics tools producing more and more “personalised” data with a fraction of the cost used to entail (Martin-Sanchez et al. 2015). This is matched with the booming use of ML and AI in Healthcare and the rapid development of “middleware” toolkits which allow biomedical researchers and clinicians to easily access and use predictive analytics tools.
(e) Since the frightening figures of healthcare errors and associated mortality/morbidity have been unveiled during the last decades [3rd leading cause of death and disability in the US] (Makary et al. 2017), new processes and methods to strengthen patient safety and to prevent healthcare associated errors are becoming issues of utmost priority. Digitisation of patient records and the booming penetration of Hospital or Specialty oriented Clinical Information Systems/Patient Data management systems could help towards this direction (Prgomet et al. 2017). However, only a single-digit fraction of USA Hospitals enrolled into the first phase of digitisation of healthcare records has entered the 2nd (HealthIT.gov). It is becoming clear that, knowledge/experience transfer from similar successful implementations like the aviation industry as well as more sophistication and introduction of Artificial Intelligence (AI) tools is the way forward. This pathway, in turn, faces serious conceptual, ethical and financial challenges (Clifton et al. 2015).
(f) Specialty-oriented clinical information systems customised to the needs of acute medical specialties and areas like A&E, ICUs, HDUs, CCUs, ORs etc. are now increasingly being replaced (or attempted to be replaced) by hospital information systems in the name and context of better integration, interoperability and cost control. Serious controversy has been developed since this trend has been enforced by hospital authorities with -frequently- very little discussion and poor customisation process. On the other hand, the arguments for an all-encompassing HIS are solid and intuitive. It is, however, widely accepted in the scientific community, though inadequately investigated, that the usability of those systems is at least sub-optimal (Dincklage et al. 2017). The community of patients, clinicians, administrators, researchers, academics, healthcare industry management shall thus find its way to meet a number of relevant challenges: i) development of acute care specialties ontology involving clinical as well as physiology/pathophysiology and organ support terminology; ii) adoption of common standards that will allow seamless integration of data from medical diagnostic, monitoring and organ support devices; iii) consensus on minimum requirements of clinical information systems functionality; iv) development of new visualisation techniques which will improve clinical decision making with documented results. It is encouraging that quality certification standards are moving towards this direction adopting the “dialogue principles” defined in the ISO standard 9241-110 as suitability for the task, suitability for learning, suitability for individualisation, conformity with user expectations, self-descriptiveness, controllability and error tolerance (sis.se/api/document/preview/907276/).
(g) Clinical education at all levels and for all students and healthcare personnel involved in acute, emergency and intensive care (physicians, nurses, physiotherapists, clinical dieticians, clinical pharmacists, clinical psychologists etc) has been always a high priority, given the complexity of the working environment and the skills required. Nowadays it enters a new era, as time and physical presence boundaries are dissolving, expertise gaps can be bridged, data access is becoming increasingly easy and modelling of diseases/procedures is revolutionised with the use of internet, telemedicine and virtual/augmented reality technologies. Globalisation and free movement of healthcare personnel as well as high demand for competence standardisation and specialisation has rendered international curricula and the role of scientific societies very important, as self-paced eLearning is booming worldwide (docebo.com).
(h) Inter-disciplinary -as opposed to multidisciplinary- approach to challenges, came through 4IR and shall stay with us! Acute, Emergency and Intensive Care is no exception but rather a wonderful example to apply and build on this concept. It is time to think big and bring help in this particularly challenging endeavour where human lives are at stake. On top of the traditional members of the ICU team, basic lifesciences scientists, psychologists, engineers, architects and bioinformaticians should find their place to our routines. Working environment in clinical areas, especially IT HIS/EHR infrastructure is expected to facilitate and provide structured, yet flexible approaches to this interdisciplinary interaction in order to maximise its impact on patient outcomes, our ultimate target!
Key points
- Acute care specialties in Europe and the world face unequivocal challenges and at the same time enjoy unprecedented opportunities amidst the rapidly changing and transformative environment of the 4th industrial revolution
- There is an ever-increasing demand for numerous forms of acute care hospital & community based- services
- Caring for the acutely/critically ill becomes increasingly complex and encompasses multiple intra-hospital transfers and interactions with numerous medical specialties and healthcare professionals
- The demand for conceptually personalised approaches to diagnosis and treatment continues to increase
- New processes and methods to strengthen patient safety and to prevent healthcare associated errors are becoming issues of utmost priority
References:
American Hospital Association Uncompensated Hospital Care Cost Fact Sheet (2017) AHA. Available from aha.org/system/files/2018-01/2017-uncompensated-care-factsheet.pdf
Asehnoune K et al. (2017) The research agenda for trauma critical care. Intensive Care Med. Sep;43(9):1340-1351.
Blum JM et al. (2015) Design and implementation of a hospital wide waveform capture system. J Clin Monit Comput, 29:359–362.
Burykin A et al. (2011) Using ‘‘off-the-shelf’’ tools for terabyte-scale waveform recording in intensive care: computer system design, database description and lessons learned. Comput. Methods Programs Biomed.
Clifton DA et al (2015) Health Informatics via Machine Learning for the Clinical Management of Patients. Year book Med Inform. 10:38-43, IMIA and Schattauer GmbH.
Dincklage F et al. (2017) Investigation of the Usability of Computerized Critical Care Information Systems in Germany. Journal of Intensive Care Medicine 1-11.
eLearning market trends and forecast 2017-2021 (2016). Available from docebo.com.
Ergonomics of human system interaction. ISO 9241-110. Available from sis.se/api/document/preview/907276/.
Evans RS (2016) Electronic Health Records: Then, Now, and in the Future. Year book Med Inform; Suppl1:S48-61, IMIA and Schattauer GmbH.
Health expenditures. Centers for Disease Control and Prevention. Available from cdc.gov/nchs/fastats/health-expenditures.htm
Halpern NA et al. (2016) Trends in critical care beds and use among population groups and Medicare and Medicaid beneficiaries in the United States: 2000–2010. Crit Care Med.Aug; 44(8):1490–1499.
Islam MDM et al. (2018) Recent Advancement of Clinical Information Systems: Opportunities and Challenges. Year book Med Inform. 83-90, IMIA and Schattauer GmbH.
Kent, J (2018) Big Data to See Explosive Growth, Challenging Healthcare Organizations. HealhtIT Analytics. Available from healthitanalytics.com/news/big-data-to-see-explosive-growth-challenging-healthcare-organizations
Makary MA et al. (2016) Analysis: Medical error—the third leading cause of death in the US. BMJ; 353.
Martin-Sanchez F et al. (2015) Medicine Possible With Real-Time Integration of Genomic and Clinical Data To Inform Clinical Decision-Making. Series Studies in Health Technology and Informatics e-book Volume 216: MEDINFO: eHealth-enabled Health.
Prgomet M et al. (2017) Impact of commercial computerized provider order entry (CPOE) and clinical decision support systems (CDSSs) on medication errors, length of stay, and mortality in intensive care units: a systematic review and meta-analysis. Journal of the American Medical Informatics Association, 24(2):413–422.
Quick Stats. Health IT Dashboard. Available from dashboard.healthit.gov/quickstats/quickstats.php.
Ridgeon E et al. (2017) The Fragility Index in Multicenter Randomized Controlled Critical Care Trials. Crit Care Med 2016 44/7:1278–1284.
Statement from FDA Commissioner Scott Gottlieb, M.D., and Jeff Shuren, M.D., Director of the Center for Devices and Radiological Health, on a record year for device innovation. FDA. Available from fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm629917.htm
Toward Precision Medicine: Building a Knowledge Network for Biomedical Research and a New Taxonomy of Disease. National Research Council, Division on Earth and Life Studies, Board on Life Sciences, Committee on A Framework for Developing a New Taxonomy of Disease. National Academies Press, Dec 16, 2011.
Wu P et al.(2017) -Omic and Electronic Health Records Big Data Analytics for Precision Medicine. IEEE Trans Biomed Eng. February; 64(2): 263–273.




















