The last 3 years have been very difficult times for healthcare organisations
as they have faced and dealt with the challenges of COVID-19, supply chain
disruptions, and staffing problems. The 2022 Digital Health Most Wired
survey, conducted by CHIME, shows how facilities are increasingly turning to
digital tools to address infrastructure, security, administrative/supply chain,
analytics/data management, innovation and other clinical and business areas.
Key Points
- The 2022 Digital Health Most Wired (DHMW) survey,
conducted annually by the College of Healthcare Information
Management Executives (CHIME), shows how facilities turned
to digital tools to address several challenges in the recent
years, including the impacts from COVID-19.
- 18 U.S. acute care organisations and 17 U.S. ambulatory
organisations achieved the highest level of recognition. Many
of them implemented advanced technologies, but they often
leverage these technologies in innovative ways and have
encouraged deep adoption across their entire organisation.
- Across the survey’s nine sections, there are numerous of
findings that show not only how care delivery organisations are
rebounding from the crises of the past several years but also
how they continue to advance their digital health agendas.
Results from 2022 Digital Health Most Wired
Survey Show Digital Trends
Healthcare delivery organisations have faced a
combination of historic global challenges over the past
several years: pandemic, supply chain disruptions, and
high inflation. These challenges have impacted clinical
and business operations with a variety of outcomes and
consequences.
These impacts are evident in the 2022 Digital Health
Most Wired (DHMW) survey, conducted annually by
the College of Healthcare Information Management
Executives (CHIME). This survey represents over
38,000 facilities from 10 countries, primary from
the United States (U.S.). Those providers include
organisations that serve patients across the continuum
of care: acute care, ambulatory care, and long-term/
post-acute care.
This year, 18 U.S. acute care organisations and 17
U.S. ambulatory organisations achieved the highest
level of recognition, Level 10. In addition to meeting the criteria for levels 1–8, organisations at level 9 or 10
are often leaders in healthcare technology who actively
push the industry forward. Not only have many of them
implemented advanced technologies, but they often
leverage these technologies in innovative ways and
have encouraged deep adoption across their entire
organisation. As a result, they are realising meaningful
outcomes, including improved quality of care, improved
patient experience, reduced costs, and broader patient
access to healthcare services. Some of the advanced
technologies used to achieve these outcomes include
telehealth solutions, price-transparency and costanalysis tools, access to data at the point of care, and
tools to engage patients and their families throughout
the care process.
Particularly related to the COVID-19 pandemic and
resulting supply chain disruptions, the survey reports
a historically high number of facilities achieving the
highest level of recognition (Level 10) in the areas of
Administrative & Supply Chain and Clinical Quality & Safety as care delivery organisations rebound from this
double hit.
Real-time insight into supply chains, product inventory,
and bed/exam room tracking is important, but the
criticality of such insight became evident over the past
several years. As a result from the disruption of supply
deliveries, unprecedented demand for clinical supplies,
and skyrocketing emergency care demand, real-time
monitoring became a paramount concern. Significant
increases were reported by the DHMW survey in the
use of bed/exam room tracking and patient-flow software
systems as compared to 2021. Among intensive care units,
an area especially hard hit by the pandemic, such tracking
system use increased by 11% over the previous year.
Bed/Exam Room Tracking or Patient Flow Software
The unprecedented patient demand, especially in the
areas of emergency and intensive care resulting from
COVID-19 related illnesses, also impacted the extent to
which care delivery facilities utilised digitally integrated
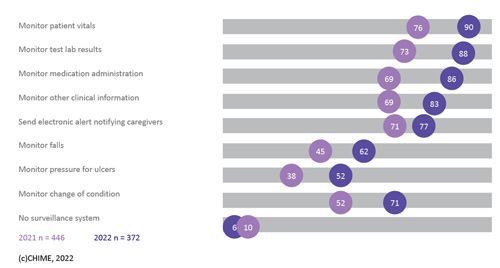
clinical tools. Digitally integrated surveillance systems
in the areas of monitoring patient vitals, monitoring test
lab results, monitoring medication administration, and
monitoring of other clinical information all increased by
20% or more over the past year.
Surveillance System integrated with EHR
These results provide two important takeaways.
First, leveraging digital technology to make the right
information available to the right people when needed
continues to be a key information technology objective.
Second, the extremely high demand for clinical care for high-risk patients further increased the imperative to
have digital tools integrating care into record keeping on
a real-time basis. Between the high demand and staffing
shortages, digitally supported care is critical to clinical
quality and safety.
Across the survey’s nine sections, there are numerous
of findings that show not only how care delivery
organisations are rebounding from the crises of the past
several years but also how they continue to advance
their digital health agendas. Areas ranging from
wireless technology to analytics & data management
to patient engagement show further adoption of digital
technologies.
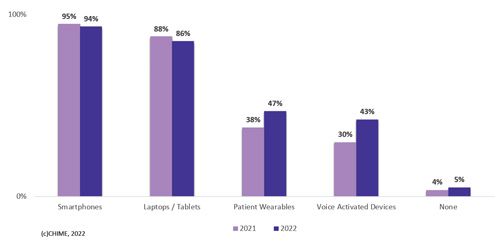
Infrastructure trends reported in the 2022 DHMW
survey show significant year-over-year increases in
mobile point of care devices (+9%) and traveling profiles
(+8%) as the demand on clinical staff rapid response
intensified during the pandemic and was exacerbated by
clinical shortages. Furthermore, use of employee-owned
devices for patient care has become near ubiquitous
with 94% of facilities allowing use of employee-owned
smartphones and 86% allowing use of employee-owned
laptops/tablets for patient care.
Adoption of Employee-Owned Devices in the Use of Patient Care
As widely promoted in trade show exhibitions and
vendor advertisements, data analytics has been viewed
as a growth area in health information technology. In
fact, the survey does show significant growth in the use
of near real-time analytics and in the delivery of data to
clinical leaders. However, there is also evidence of gaps
in adoption and level of sophistication.
Foundational components for clinical and business
analytics, enterprise data warehouses (EDW) or
operational data stores (ODS) exist in 94% of the
responding facilities for their clinical and business
intelligence efforts. But what is housed there varies:
69% send supply chain/ERP data to the EDW or ODS
while only 39% send CRM data there. The survey
also found that clinical quality metrics were the most
commonly delivered for real-time analytics while only
45% delivered data related to social determinants of health.
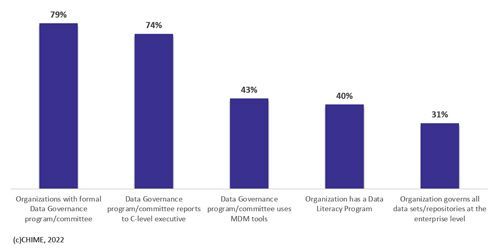
Style of data governance and use of data
governance tools provide an insight into the level of
data management sophistication for care delivery
organisations. While 79% of respondents have
established a formal data governance program/
committee, just 43% of them use master data
management tools and only 31% govern all data sets/
repositories at an enterprise level. This illustrates the
evolution still ahead for most care delivery organisations.
Adoption and Execution of Data Governance Program
Not surprisingly in this pandemic era, digital tools to
remotely connect and engage with patients show some
of the largest increases reported. Increasingly, care
delivery organisations are creating dedicated digital
officers to drive their digital health strategies which are
often focused heavily on engaging patients outside of
the facility. The survey reported 16% increases in the
use of patient/family facing videos to educate patients
and to share lab and test results and an 11% increase
in such videos to address medication prescriptions and
related matters.
Conversely, as the 2020 and 2021 hospitalisation
spikes were replaced by somewhat smaller spikes in
2022, telehealth visits among reporting facilities declined
by nearly 6% to just 13% of total visits. Particularly in
the United States where payment methodologies may
influence visits, there remains much to be done to drive
care to the most effective, most efficient, and most
convenient locus of care.
A new section to the 2022 DHMW survey focused on
innovation. Investments in new technologies and digital
solutions are clear drivers of innovation. While the ability
to pursue such investments is affected by the resources
available for such purposes, nearly all reporting
organisations (96%) are looking to drive clinical
innovation through investment in these solutions. More
than 23% of all reporting organisations expect to spend
10% or more of their IT spend on experimentation/trials
of technological innovation, new ideas, ventures, and
related solutions. This illustrates not only how important investing in innovation is but also how many are
aggressively pursuing these strategies to improve their
ability to deliver care and achieve optimal outcomes.
So where does this level of investment put health
care organisations on their transformational journey?
Sixty-eight percent report they are on or ahead of
their schedule in their digital transformation execution,
compared to plan with the biggest challenges to
realising a successful transformation being a lack
of dedicated budget (20%), cultural resistance
(15%), tendency for short-term planning over longterm planning (12%), and an over reliance on legacy
technology (11%).
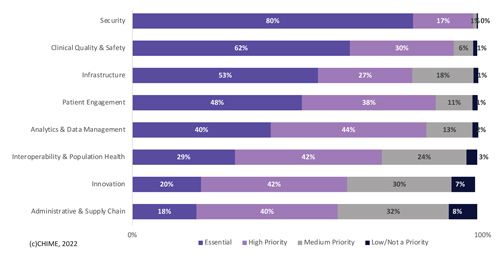
Organisational Priorities for 2023
Finally, the survey also asked participants to identify their organisational priorities for 2023. The highest
reported priority, with 97% classifying this as an
essential or high priority, was security. This was followed
closely by clinical quality and safety with 92% rating this
area as an essential or high priority and the third most
important priority for 2023 by these respondents was
patient engagement at 86%. All are consistent findings
with expectations held by most and despite heavy focus
and investment in these areas over the past few years,
they remain at the top of most priority lists.
The primary survey is conducted each year between
April and June; however, organisations may contact
CHIME at any time to receive the current year’s survey
instrument and submit their data for scoring.
For more information, go to https://dhinsights.org/
analytics and click on the I Am A New Provider Partner
button. More detail on the 2022 Digital Health Most
Wired survey can also be found in the National Trends
Report which is available at
https://dhix.dhinsights.org/wp-content/uploads/2022/11/2022-DHMW-NationalTrends-Report.pdf.
Conflict of Interest
I am on contract with CHIME as their Chief Analytics
Officer but I have no conflict or derive no financial gain
from the publication of this article