HealthManagement, Volume 24 - Issue 4, 2024
As the population ages and chronic diseases rise, healthcare systems increasingly turn to virtual and remote care to meet growing demands. These innovations transform patient outcomes by enabling preventative care, offering personalised treatment and reducing hospital readmissions. Applied across a wide range of medical fields, virtual care helps address critical healthcare challenges. However, overcoming obstacles such as regulatory frameworks, data security, and integration remains key to fully unlocking these innovations’ potential.
Key Points
- Healthcare systems are increasingly adopting virtual and remote care to address the challenges of ageing populations and rising chronic diseases.
- These technologies enhance care in mental health, cardiology, oncology, and wound care by reducing hospital readmissions and enabling timely interventions.
- Virtual care focuses on preventive care and allows for more personalised treatment, enabling patients to receive care at home.
- While AI and digital therapeutics are transforming healthcare, issues like data security and regulatory hurdles remain.
- Telemonitoring and AI-driven tools are set to significantly improve healthcare efficiency, patient care, and accessibility.
As the global population ages and the prevalence of chronic diseases rises, healthcare systems worldwide are increasingly turning to virtual and remote care as indispensable tools. These innovative approaches are crucial in addressing the challenges of an ageing population and rising chronic diseases. They help sustain healthcare delivery and drive significant improvements in patient outcomes. By focusing on prevention and enabling patients to receive care in the comfort of their homes, virtual and remote care contribute to a more personalised and positive healthcare experience. This article explores how these technologies are applied across various medical fields, from mental health and cardiology to oncology and wound management. Virtual mental health consultations are expanding access to care, especially in underserved areas, while heart failure telemonitoring is reducing hospital readmissions and improving patient management. Oncology remote monitoring enables timely interventions, and wound management remote care is cost-effectively optimising treatment outcomes. Furthermore, the emerging field of digital therapeutics is on track to transform the way chronic conditions are managed, offering tailored, data-driven solutions.
To provide practical insights into these advancements, Thierry Godelle interviewed leaders in telemedicine, remote patient monitoring (RPM), and digital therapeutics (DTX) across these clinical domains. They shared the encouraging trends in the adoption of these solutions and highlighted the challenges that must be overcome to fully realise their potential in transforming healthcare delivery. These challenges include data security, interoperability, and regulatory frameworks. Overcoming these hurdles is needed to ensure the widespread and effective implementation of virtual and remote care technologies.
Remote Patient Monitoring (RPM) of Heart Failure Patients
In 2021, Oliver Piepenstock, Marcus Hott, and Leonhard Riehle established Noah Labs in Berlin with the ambitious goal of revolutionising cardiology through artificial intelligence. Their flagship product, Noah Labs Ark, is a state-of-the-art remote monitoring solution tailored specifically for heart failure patients. What sets Ark apart is its proactive monitoring of key biomarkers, enabling early detection of deterioration. This unique feature positions Ark as a promising tool in managing heart failure, as it can stabilise patients and prevent hospital admissions.
Progress in Virtual and Remote Care for Heart Failure Patients
Oliver Piepenstock highlights the substantial progress made in Europe regarding virtual and remote care for chronic conditions such as heart failure. Programmes like France’s ETAPES and Germany’s TIM-HF1 and TIM-HF2 studies have demonstrated the transformative impact of integrating virtual care elements into treatment pathways. These studies have shown that virtual care can significantly reduce hospitalisations and mortality rates. This success paves the way for the broader adoption of such technologies, provided that supportive policies, reimbursement structures, and guidelines are in place. France, in particular, has been at the forefront of expanding virtual care across various medical conditions, setting a precedent for other European countries to follow.
Hospital Adaptation and Telemonitoring Trends
As telemonitoring becomes more prevalent, hospitals adapt their practices to integrate these technologies. In Germany, hospitals have increasingly acquired outpatient practices to benefit from outpatient reimbursement schemes. Though primarily targeting outpatient care, telemonitoring is becoming integral to hospital systems. With their extensive infrastructure, large hospital networks are ideally positioned to manage telemonitoring on a large scale, centralising these efforts in specific facilities to ensure consistent care across regions. Financial incentives, such as reducing costly readmissions and enhancing brand loyalty, drive hospitals to embrace telemonitoring. Similar trends are seen in other European countries, including the Netherlands and Austria, where hospitals play a central role in telemonitoring within more integrated healthcare structures.
Technological Advancements and Challenges
Technological advancements are significantly reshaping telemonitoring and patient care management. Early systems required manual data recording and human decision-making, but today’s AI-driven solutions, like Noah Labs Ark, offer real-time data analysis and actionable recommendations. Innovations such as Noahlabs' Vox, which utilises voice recognition technology to monitor vital signs, exemplify the progress in predictive healthcare. These advancements improve patient outcomes, reduce costs, and enhance accessibility for facilities with limited infrastructure. Despite these benefits, challenges remain, including patient technological proficiency and inconsistent infrastructure. Addressing these issues, by exploring passive technologies or ensuring robust data transmission, is crucial for making virtual care more inclusive and seamlessly integrated into the healthcare system.
Teleconsultation in Mental Health
The Evolution of Virtual Mental Health Care
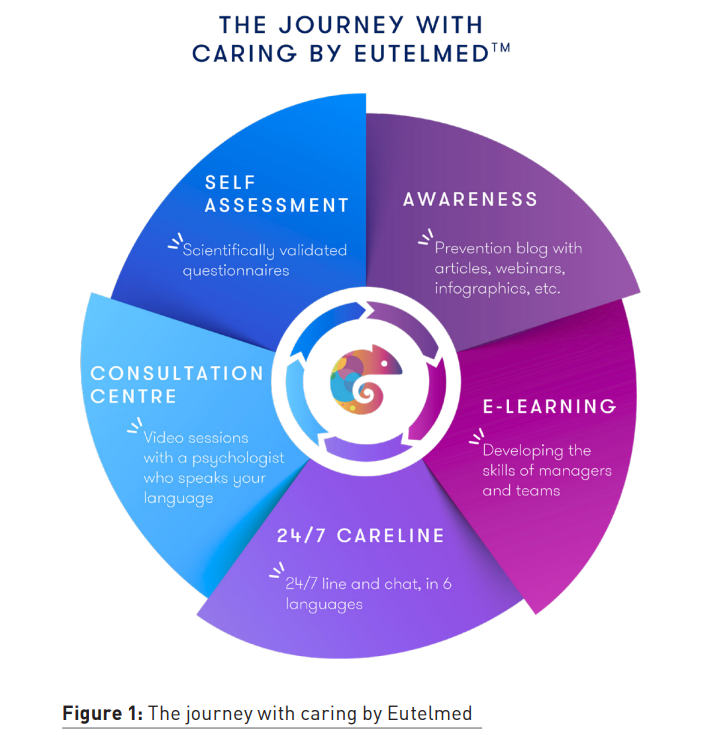
In a recent discussion with Marie-Laure Bry, Medical Director at Eutelmed, she discussed the rapidly advancing field of virtual mental health care. This sector has seen significant progress, particularly since the COVID-19 pandemic. Eutelmed, a pioneer in mental health teleconsultation since 2012, offers a unique perspective on remote mental health services' current state and future prospects. The pandemic was a significant catalyst for the widespread adoption of teleconsultations, as physical visits became restricted and people turned to virtual consultations out of necessity. This shift not only expanded access to mental health care but also helped reduce the stigma surrounding it. Virtual consultations are often perceived as less intimidating than traditional in-person visits, making it easier for people, especially younger generations who are comfortable with digital tools, to seek help.
Benefits of Mental Health Teleconsultation
Marie-Laure highlighted several advantages of teleconsultation in mental health care. One difference with in-person consultations is the increased sense of intimacy it can create between patients and practitioners. By conducting sessions in patients' personal spaces, virtual consultations may facilitate more open discussions on some personal topics—something that can be challenging to achieve in a conventional clinic setting. Teleconsultations also offer continuity of care for individuals who travel frequently or live far from home, allowing them to maintain regular mental health support without needing to travel. This ensures ongoing care and follow-ups regardless of the patient's location or medical deserts, particularly for psychiatry, which is becoming a rare and sought-after medical service. Additionally, Eutelmed’s commitment to providing services in over 60 languages addresses both language and cultural barriers, ensuring culturally sensitive care that meets patients' specific needs. The company has also developed a comprehensive digital physical and mental health assessment tool available in 20 languages, which helps identify risk and protective factors and guide targeted in-person consultations if necessary.
Challenges and Innovations
Despite the numerous advantages, teleconsultation in mental health faces several challenges. Marie-Laure noted the need for clear regulations governing cross-border teleconsultations, especially regarding medication prescriptions and adherence to global data protection standards like GDPR. The absence of standardised regulations complicates international consultations and can impact the effectiveness of telehealth services.
Another concern is the potential for increased patient isolation. As more aspects of life are managed online, there is a risk that individuals may become more socially isolated, which could negatively affect their mental health. Additionally, issues with internet connectivity can limit access to telehealth services, particularly in rural or underserved areas.
Marie-Laure also discussed several promising innovations in the field. Vocal biomarkers, which aim to detect or estimate the severity of psychological distress and mental health disorders through vocal patterns, are a significant advance still in the development phase. These biomarkers could enhance teleconsultations by providing additional clinical insights.
Conversational chatbots are another innovation being explored to offer ongoing support between consultations, maintain patient engagement, and address concerns outside scheduled sessions.
AI-driven tools are already being used to assist with administrative tasks such as drafting medical reports, potentially streamlining processes and improving care efficiency by increasing the exchange time between patient and doctor.
However, Marie-Laure emphasised that while these technologies offer exciting possibilities, they should complement rather than replace the essential human connection in mental health care. The ultimate goal is to enhance the patient experience with digital tools while preserving the core human element crucial for effective therapy.
Balancing Human Interaction and Virtual Care for Mental Health Patients
Virtual mental health care has evolved rapidly, driven by necessity and innovation. While virtual care offers substantial benefits, such as reduced stigma, increased accessibility, and better continuity of care, it also presents challenges, including regulatory issues, potential patient isolation, and connectivity barriers. Innovations like vocal biomarkers and conversational chatbots hold promise for the future. Still, balancing these technological advancements with the irreplaceable value of human interaction in mental health care is essential.
Digital Solutions Aid Mental Health’s Transformative Shift
Virtual care in mental health is on the cusp of a significant transformation, driven by advancements in technology that address longstanding challenges in diagnosis, treatment, and patient management. To gain deeper insights into this evolving landscape, I interviewed Tanel Petelot, founder and CEO of Emobot. His perspective sheds light on how innovative digital tools are revolutionising psychiatric care, offering a promising glimpse into the future of mental health treatment.
Addressing the Gaps in Mental Health Care With Virtual Care
Emobot, founded in April 2022, is making waves in the mental health field with its focus on the objective evaluation of mood disorders such as bipolar disorder and depression. These conditions affect 20-25% of the general population but remain poorly understood and inadequately treated. With a third of patients not responding to current therapies, the complexity of mood disorders—intersecting biological and psychological factors—challenges the efficacy of treatments based solely on pharmaceuticals. Traditional diagnostic tools are often inadequate, exacerbating difficulties in treatment due to a limited understanding of these disorders.
In France, the disparity between the number of psychiatrists and the growing patient population is glaring, with 3.2 million patients on antidepressants and only 15,000 psychiatrists. This imbalance results in long waiting times, sometimes up to four months, particularly for young people. The situation has been further aggravated by the COVID-19 pandemic, highlighting a critical need for more efficient and accessible mental health care solutions.
Emobot’s Innovative Approach with EmoDTx
Emobot’s solutions address these issues by developing technology that continuously measures patients' emotions, providing passive and objective data on their emotional state. This data aids doctors in diagnosing and adjusting treatments while also empowering patients to understand better and manage their moods. The company is also integrating digital therapies into its offerings in collaboration with hospitals in Germany. This integration, EmoDTx, associates mood monitoring with real-time personalised cognitive behavioural therapies, aiming to provide personalised and effective care, with around a hundred psychiatrist partners and ongoing clinical studies for approval in Germany. By enhancing both accessibility and effectiveness, Emobot is at the forefront of a paradigm shift in psychiatric care.
Navigating Challenges and Opportunities of Digital Solutions for Mental Health Care
Despite the potential benefits, integrating digital solutions into mental health care presents several challenges. One significant issue is patient engagement, particularly for those suffering from depression, where motivation can be a barrier. Digital tools, while promising, must be designed to avoid further discouraging patients. Tanel emphasised that careful design and thoughtful strategies are crucial to ensuring these tools are effective and engaging.
Another challenge is the generational divide among psychiatrists. While many younger practitioners are open to incorporating digital tools, older generations trained in traditional psychoanalytic methods may resist such changes. This divide can create institutional hurdles, particularly in decision-making bodies dominated by older practitioners.
Additionally, digital therapeutics offer a promising alternative to traditional medications, often insufficient or poorly adhered to by patients. Digital solutions provide a lower-cost, more accessible, and engaging approach to treatment, making mental health care more reachable for underserved populations while addressing some of the limitations of conventional therapies.
Virtual mental health care is undergoing a significant transformation, driven by technological advancements and accelerated by the COVID-19 pandemic. Companies like Eutelmed and Emobot are at the forefront of enhancing accessibility and personalising care. Eutelmed’s teleconsultations have expanded access and reduced stigma, while Emobot’s Emo-DTX technology provides objective data to manage mood disorders better.
Despite the progress, challenges remain. Ensuring patient engagement, particularly among those with depression, requires careful tool design. Additionally, the generational divide among psychiatrists can create institutional hurdles. Yet, innovations such as vocal biomarkers and AI-driven tools offer promising solutions. Overall, integrating digital solutions into mental health care holds great promise. Balancing these technologies with essential human interaction will be key to achieving effective and transformative mental health treatment.
Wound Care
After examining virtual care advancements in heart failure and mental health, it's essential to address wound management, which warrants its own focus due to its distinct complexities. Unlike other specialities, wound care involves diverse, interdisciplinary treatments and specific monitoring needs that differ significantly from chronic disease management or mental health support. Virtual care in wound management requires specialised tools to handle detailed documentation and real-time assessments, addressing challenges unique to this field. By exploring this area separately, we wanted to share insight into how tailored digital solutions can optimise wound care, enhance efficiency, and improve patient outcomes.
Integrating Remote Care Solutions in Hospitals
In my discussion with Matis Ringdal, CEO of Pixacare, a Strasbourg-based remote Wound Care application, several crucial insights emerged about integrating remote care solutions into hospital settings and their influence on clinical practices. Matis emphasised that adopting remote management technologies requires a tailored approach to meet the unique needs of different medical specialities. While the COVID-19 pandemic accelerated the adoption of these technologies, their success hinges on aligning them with the specific workflows of each department, such as cardiology or surgery. A one-size-fits-all strategy is inadequate due to each speciality's distinct demands and challenges. Effective integration requires addressing these unique needs to ensure that remote care solutions enhance rather than disrupt existing practices.
Challenges and Solutions in Remote Care Adoption
Matis highlighted several challenges in adopting remote care technologies, including regulatory hurdles and the need to maintain essential human interaction. Remote care solutions must adhere to regulatory standards while complementing existing care structures without causing disruptions.
Furthermore, Matis pointed out that AI-driven tools have the potential to enhance traditional care practices rather than replace them. Pixacare's focus on wound care management exemplifies the complexity of integrating remote care. Wound care often spans multiple disciplines, leading to inconsistencies in treatment due to varying expertise and approaches. Traditional documentation methods, reliant on paper forms and manual measurements, introduce variability and communication issues among providers.
Pixacare’s Innovative Approach to Wound Care
Pixacare addresses these challenges with a platform that standardises wound documentation and facilitates collaborative care. Clinicians use the platform to photograph wounds, automatically document their size, and track healing progress over time. This remote monitoring capability allows for asynchronous wound assessment, enabling quicker responses to worsening conditions.
By reducing hospital visits and improving communication among healthcare providers, Pixacare's solution enhances healing by 30%, lowers costs, and streamlines the care process. Currently operational in 30 hospital sites across France, including major academic hospitals and cancer centres, Pixacare’s technology serves over 90,000 patients.
Because of the current lack of reimbursement, the company employs a B2B model to secure earnings, providing its solution directly to specialised wound care centres. Matis stressed the importance of securing reimbursement to expand market reach, aiming to democratise access to remote monitoring by integrating reimbursement models similar to those for chronic conditions like diabetes and heart failure.
Future Prospects and Strategic Expansion of Pixacare
Pixacare plans to expand its operations beyond France into other European markets, including Germany, the Nordic countries, and the UK. These markets are more mature and receptive to telemonitoring. Matis mentioned the upcoming potential for integrating paramedical support through external platforms to enhance patient monitoring and data documentation. For now, Pixacare remains focused on advancing technology, ensuring regulatory compliance, and securing reimbursement.
The company is also open to future collaborations with healthcare service platforms to further its mission of improving remote care. In summary, Pixacare’s approach underscores the importance of customising remote care solutions to meet specific clinical needs, overcoming barriers to adoption, and strategically expanding market presence. The company's innovative platform addresses critical inefficiencies in wound care management, significantly improving patient outcomes and operational efficiency.
Current State and Future of Virtual and Remote Care
Today, telemedicine is advancing on multiple fronts, thanks to critical improvements in hospital workflows, integration between hospital and community care, and financial and patient-related aspects. Key developments include customising telehealth solutions to meet the specific needs of different medical specialities. Telemedicine technologies are increasingly being integrated with existing care systems, which enhances efficiency while minimising disruptions to traditional processes.
To better understand the outlook of Virtual and remote care, I interviewed Axel Pilicer who founded GutyCare, one of the first French Digital Therapeutics solution that was eventually integrated into Résilience, a leader remote patient monitoring solution editor for cancer patients. From where he sits, Axel is ideally positioned to observe and analyse where virtual and remote care currently stands and how it should evolve in France, Europe and globally.
As Axel shared, the accelerated adoption of telemedicine has been driven by better workflow management, simplified interactions between remote and in-person care, and evolving financial models such as developing reimbursement options, as we already saw in particular for heart failure patients. Additionally, educating healthcare professionals about the benefits and use of new technologies has been crucial in this process. However, challenges remain, including regulatory hurdles, integration with existing systems, and the need to maintain essential human interactions. To fully realise the potential of telemedicine, it is crucial to address these barriers and continue improving the patient and provider experience.
GutyCare: CEO’s Axel Pilicer testimonial on launching and developing a digital therapeutics solution in France:
“We developed a device to monitor patients with chronic illnesses, predict adverse events and relapses, and support home care through a Digital Therapeutics (DTX) module, which includes nutrition and psychological support beyond just treatment. These solutions complement each other well. After extensive development, we pursued both fundraising and a potential sale to Résilience. Ultimately, we completed our fundraising in 14 months and decided to sell, given the complex market conditions and the realisation that the startup landscape had become less favourable.
Raising funds in this field is challenging, particularly before securing reimbursement from health insurance. In France, RPM (remote patient telemonitoring) is more advanced than in Germany, where Digital Therapeutics (DTX) is gaining traction but faces high barriers to entry. While telemonitoring is progressing and achieving reimbursement milestones in France, DTX is still in its early stages and has seen limited success. For instance, Resilience is the first company in France to receive reimbursement for a telemonitoring solution in oncology as it has reached a level of maturity that is not common in the market where DTX remains underdeveloped and still faces many hurdles. Overall, the market for DTX in France is evolving slowly, with many companies needing to prove their effectiveness and secure funding before achieving widespread adoption.”
Integration of Telemonitoring in Healthcare Facilities
Axel concurs that telemonitoring has the potential to significantly impact healthcare systems, mainly by reducing hospital congestion, saving time for medical staff, and lowering costs. This appeal is particularly relevant to hospital directors and managers. The core goal is to predict falls, adverse events, and complications before they occur, thus streamlining patient care and easing the burden on healthcare facilities. However, integrating these solutions is challenging. For telemonitoring systems to be successful, they must be user-friendly and efficiently integrated into existing workflows. Past failures often stemmed from solutions that were either too complex or not adequately adapted to user needs despite passing clinical studies.
Several factors influence the speed and success of telemonitoring adoption. For instance, healthcare professionals may resist new technologies if they perceive them as time-consuming or if they don’t clearly benefit their daily routines. Therefore, it's crucial to demonstrate that these solutions will save physicians time while improving patient care. Effective integration requires ongoing support to address technical issues and adapt to evolving needs, while regulatory constraints (namely revalidations of the solution) can slow down necessary improvements.
Patient acceptance is another hurdle. Solutions must cater to diverse patient populations, including elderly individuals who might be less inclined to use new technologies. Ensuring patients understand the benefits and feel comfortable using the technology is also essential.
Overall, successful telemonitoring solutions must balance usability with regulatory compliance and demonstrate clear benefits to both healthcare providers and patients. When well-designed, these systems can lead to a more efficient, cost-effective healthcare environment where all parties benefit.
Facilitating the Adoption of Telemonitoring and Digital Therapeutics
For telemonitoring and digital therapeutic solutions to be effective, healthcare providers and patients must fully engage with them. Success hinges on overcoming several hurdles related to usability and integration.
According to Axel, these solutions must offer clear value and be easy to use. A key challenge is ensuring physicians and patients are willing to adopt these technologies. Physicians often face scepticism about new tools due to the overwhelming number of digital solutions they encounter and their already heavy workloads. To address this, digital solutions must seamlessly integrate into existing systems, be straightforward, and clearly demonstrate how they save time and improve patient outcomes.
For physicians, avoiding a fragmented experience across multiple portals is crucial. Ideally, digital tools should not add to their already complex workflow but should instead simplify their tasks. An effective strategy could be integrating telemonitoring data into existing medical record systems or using simple communication methods like SMS for patient updates. The goal is to make the process as streamlined and intuitive as possible, avoiding additional complexity.
On the other hand, patients need solutions that are easy to use and demand minimal effort. Many patients, especially those with chronic conditions, prefer simplicity. Complex systems or demanding processes can lead to disengagement. Solutions that offer easy-to-navigate interfaces and require minimal input from the patient, such as SMS-based questionnaires, are more likely to be embraced.
Both telemonitoring and digital therapeutic tools should be designed with a focus on user experience (UX). Drawing from successful consumer applications can guide the creation of user-friendly, practical solutions. Balancing comprehensive content with ease of use is critical; overly complex systems can deter users, while overly simplistic ones may not meet clinical needs.
Ultimately, the success of these digital tools depends on their ability to integrate seamlessly into healthcare practices and provide a user-friendly experience for both patients and providers. Digital solutions can better address real-world needs and facilitate wider adoption by focusing on simplicity and direct value.
Future Outlook for Digital Health Technologies
The digital health sector is expected to experience significant evolution and growth in the coming years. Here’s how Axel envisions the landscape unfolding over the next 12 months and the next five years:
Short-Term (Next 12 Months):
- Acceleration and Integration: Adopting digital health solutions, including telemonitoring and digital therapeutics (DTx), is set to accelerate. Solutions that initially faced scepticism, such as the DIGA in Germany, are gradually gaining traction as their effectiveness becomes clearer.
- Standardisation: Digital health solutions will likely become more standardised, moving from niche applications to common practices in healthcare. This includes both telemonitoring and DTx becoming routine tools rather than specialised or "gadget" solutions.
- Emergence of Leaders: The competitive landscape will see the rise of key players who establish themselves as leaders in the field. These leaders will likely drive innovation and set standards.
Medium-Term (Next 5 Years):
- Consolidation and Dominance: The sector will likely undergo significant consolidation. Smaller or less effective startups may struggle to survive, leading to the dominance of a few large players. These leaders could become akin to "digital pharmaceutical companies," managing multiple digital health assets.
- Integration with Traditional Healthcare: Digital health technologies will increasingly be integrated into traditional healthcare systems. Tools like AI-driven diagnostic aids and telemonitoring will become standard components of patient care, complementing rather than replacing human expertise.
- Increased Automation: With advancements in AI and machine learning, symptom tracking and disease management automation will become more sophisticated. This will help reduce costs and improve patient care by offering timely and personalised interventions.
Long-Term Vision:
- Health Tech Giants: In the long term, digital health giants may emerge, potentially rivalling or surpassing traditional pharmaceutical companies in valuation and influence. These companies will likely have expansive portfolios of digital health products and services.
- AI and Data Utilisation: AI will be crucial in driving the next wave of innovation, enhancing diagnostic accuracy, treatment personalisation, and operational efficiency. Integrating AI into digital health solutions will facilitate faster and more accurate decision-making, further pushing the boundaries of what's possible in healthcare.
Overall, the sector is primed for rapid growth and transformation. The key to success will be navigating the integration challenges, maintaining simplicity and usability, and leveraging technological advancements to enhance patient care and operational efficiency.
Conclusion
As the global population ages and chronic diseases rise, virtual and remote care are becoming crucial for managing increased patient loads and clinical demands. These innovative approaches enhance patient outcomes by focusing on prevention and providing care at home, leading to a more personalised healthcare experience.
This article examines how virtual care is transforming various fields: mental health consultations and digital diagnostic and therapy solutions are expanding access and reducing stigma; heart failure telemonitoring is lowering hospital readmissions; remote oncology monitoring enables timely interventions; and virtual wound care improves treatment efficiency and cuts costs. Digital therapeutics are also on track to revolutionise chronic disease management.
Interviews with virtual and remote care leaders reveal promising trends and challenges, emphasising the need for tailored solutions, effective integration, and overcoming regulatory and engagement barriers. The future of digital health looks toward accelerated adoption, greater standardisation, and seamless integration with traditional care, promising significant improvements in patient care and healthcare efficiency.
Conflict of Interest
None.



